Schizophrenia Relapse: Real Life and On "Perception", Season 2
This month we are living with fingers crossed.
Ben has had a close call, once again, with his symptoms of schizophrenia. We don't know how it happened, but somehow in late May Ben's med levels began to drop. We saw the usual warning signs (agitation, self-talk, lack of focus, too-forced interactions, loud and constant music in his iPod, lack of desire to engage, etc.) and yet he kept insisting he was "fine" and "nothing is wrong."
But we knew. And we ordered tests. The test result? Med levels near to zero.
So we took new precautions, which unfortunately must include a lockbox for the meds. It feels like we have gone backwards in the quest for Ben's independence. And ours.
What is the Cost of Schizophrenia Relapse?
For us? Trust level has dropped, supervision level must rise, and fears about Ben's future have increased. But we're used to the roller coaster ride. We've managed it before, we're managing it now, albeit with disappointment. Ben seems to be back on track, and we remain grateful for days that are productive and hopeful. Grateful - and, of course, also guarded.
But what was the possible cost for Ben? The results are coming in now - in his job (he was close to being fired, as he was acting so strangely and customers were complaining), at school (for the first time in years, he did not complete one of the classes he took, and his financial aid could be endangered), and with his friendships (he became withdrawn, and his friendships only survived because the guys came to us to find out what was happening, and were willing to understand and wait for improvement in Ben).
Ben came this close to losing everything he has worked so hard to build - all in the space of one period of medication non-compliance, however it happened.
And now? We wait and see. And lock up the meds.
How Real are the Results of Schizophrenia Relapse on Perception?
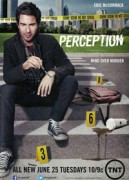 On the TV series Perception, neuroscience professor Daniel Pierce (played by Eric McCormack) lives with paranoid schizophrenia, which often conveniently manifests as helpful voices which help him solve crime. In between cases, he manages to lecture to his college students quite coherently and entertainingly.
On the TV series Perception, neuroscience professor Daniel Pierce (played by Eric McCormack) lives with paranoid schizophrenia, which often conveniently manifests as helpful voices which help him solve crime. In between cases, he manages to lecture to his college students quite coherently and entertainingly.
When not in "focus mode", though, Pierce is bothered by hallucinations and often relies on his assistant , Max Lewicki, to help him keep his realities straight. FBI Agent Kate Moretti, his partner-in-solving-crime, also keeps an eye out and sometimes asks, "Daniel, are you having an episode?". And now, the character Natalie Vincent(voice)/Dr. Caroline Newsome (real) observes Dr. Pierce having symptoms of relapse.
Of course, Pierce always answers, "I'm fine."
That's the problem - and so it is in our family.
I wrote about this series when it premiered last year, and now in Season Two, Dr. Pierce has returned from a psychotic break (at the end of Season One), hospitalization, and nine months of staying on his meds. As we pick up the show, he has stabilized enough to even begin a relationship. Things are good. But they don't stay that way for long. Pierce believes he is developing tardive dyskenisia (rare with the schizophrenia medications he is on, newer atypical anitspychotics) and weans himself off, without consulting his psychiatrist. In fact, he no longer shows up for treatment.
That, at least, is all too real to us. And some of what happens to Pierce as a result also rings true, in ways - but we have to see if his non-compliance has any more devastating results, as it has had in our family. So far, the character has held on to his job, and his friends - but he has lost his girlfriend.
So we'll keep watching. It's not a fairy tale, so that's good. And I think the writers are trying to be true to the facts of schizophrenia treatment. Pierce's case may be closer to that of those living with schizophrenia with more success in functionality than Ben has had so far. (e.g. Elyn Saks, author of The Center Cannot Hold).
But, for us, the results of a relapse are far more devastating at this point. So we keep close
[caption id="attachment_1526" align="alignright" width="170" caption="meds under lock and key"] [/caption]
[/caption]
watch. And hope the day will come when Ben can accurately gauge his own progress and relapse.
No matter what you call it - relapse, return of symptoms, regression - one of the most difficult aspects of chronic illness is the need for constant watchfulness for signs of recurring symptoms, while trying to enjoy the good days of stability.
When you add the word "mental" in front of "illness", often the ones who monitor those signs are outside observers - family, friends, and professional caregivers - because the nature of mental illness often obscures the ability to self-observe with accuracy.
APA Reference
Kaye, R.
(2013, July 5). Schizophrenia Relapse: Real Life and On "Perception", Season 2, HealthyPlace. Retrieved
on 2026, March 10 from https://www.healthyplace.com/blogs/mentalillnessinthefamily/2013/07/perception-season-2-monitoring-for-return-of-symptoms
Author: Randye Kaye
My 21 year old son was recently diagnosed with Schizophrenia due to a psychotic episode that landed him in jail and then a mental hospital after he tried to attack my husband with a knife. He is currently on medications while in the mental hospital and he is going to be released soon. My husband understandably is not wanting my son to come back and live with us and is convinced that despite medications, my son will relapse and his life is once again in danger. I am in the middle and not sure what to do. I believe just by talking to my son that the medications are helping him immensely. I can have an actual conversation with him with out him rambling and hearing voices. My son as of right know is trying to decide between pills and shots and I have been encouraging him to take the injections due to the fact I have no idea what his living situation will be like and that pills can be "lost" or forgotten. I am looking forward to the release of my son but fear my marriage and home life. Wish me luck.
Hi Randye,
I take Risperdal. I do not mind taking it per se, but it has given me ileus (paralysis of the intestinal tract, constipation). I take a low dose of medication but I still have this problem since my med is anticholinergic. So far, I have not found an agreeable med. I wish that those who insist high dose meds are the only course of action could be a little more sympathetic to the often dire consequences of taking the medications. The side effects can sometimes be devastating. I tried Haldol and while it appeared that I was "better" in fact I felt like a complete zombie which was a tortuous experience. Perhaps your son needs more insight about his illness. Is he in denial? A little empathy about struggling with a diagnosis, and compromise, goes a long way. Maybe his dosage is just too high to be tolerable.
Hi Cheryl, and thanks so much for sharing your perspective with us. The side effects are, I believe, a major reason that many go off meds, no matter what the diagnosis. That's why research and development are so important. One of the most valuable things I've learned along the way is not to "judge" Ben's desire to go off meds. I get it, I do. But I have seen the consequences, and I think Ben is closer to seeing them too. This is his journey, to acceptance, and I can't rush it for him.
That said, we ate both thrilled that right now, stable on his meds, he is working, going to school, active physically and socially, and (something he says is the number one thing) out of the hospital. He has even lost much of the weight he. Gained, by eating fewer processed foods and exercising more. All of this takes times, and I'm grateful we have had the time to allow progress to flow. Two days off meds, tho, and it all falls down like a game of Jenga when you finally pull out the supporting piece!
Thanks again so much for writing, and I wish you so many good things.
Randye
It is comforting to know that there are others who walk this road with a MI loved one. My son had a break with reality about 12 years ago he received treatment for about a week and then refused any more meds. And he got better. Bought a home, got back into college and was doing well. But that's over now. He became recluse over the last year and finally revealed to me that none of that stuff ever went away. He is now 32. Undiagnosed and untreated. He refuses any treatment. Still holds his job but only because it is a family business. He is an adult and he exhibits severe negative symptoms more often than not. It's been 4 months since he revealed all of this to me. I've contacted NAMI, it's hard for me to attend their meetings because of my work schedule. I've bought the book "I'm not sick and I don't need help".
It has helped me partner with him better and build trust. I've seen my own therapist for my own support. I am immersed in grief, worry, and guilt that I didn't see it earlier. I go by his home no less than once a week (usually more). I make sure he is eating and I try to be his one person he can count on. He's gone it alone and his it well. Telling me I am sure was a cry for help. But he refuses help all the same. So for now, all I know to do is stop by regularly and hope he will seek help. I've provided him with all the names and numbers. I won't give up. I can't. Like all of our children he is exceptionally bright and talented. It's a hard road for all of us. But his road is harder! And I am so grateful for the dialogue here. Thank you.
Hi Peggy,
I can so relate to your story, and wish you continued strength and love. Very few know what families go through when schizophrenia hits, which is why I did my best to represent us all with my family story in "Ben Behind His Voices", and here. I'm so glad this dialogue has, at least, made you feel less alone. There are so many who, unfortunately, know just hoe you feel - and continue to fight as best we can through the helplessness that comes with an illness that comes with lack of insight and refusal of treatment.
Best wishes, and lots of hugs,
Randye
Thank you for sharing your stories about your son ...my son also hates taking all the medications daily...but he will go every 4 weeks for his injection of haldol..it has been a life saver for our family. We are just past one year with no relapse and getting better daily ...bless you and your family in your journey ..we all have our daily struggles with our children.
Carmen, that's terrific news! Yes, the injectibles can be an awesome treatment choice. There is also Maintena, a new injectible of Abilify. Readers have written to share success with that one as well!
Treatment is individual, of course, and each person's case is different. My only "platform" re meds is: find the one that works for you (or your loved one) --- for lifestyle as well as results. And the more these options are developed and available, the more hope we can have.
So glad your son is doing well!
Randye
Hi Randye!
I'm dealing with the same situation, but in the opposite way. I had to secure meds in a lock case, but to prevent an abuse of some, rather than a non-compliance with the plan, for example: clonazepan. When I ask her, she always says: Yes, I took the meds as plan and no more. Or say that she was agitated and clonazepan helps her to calm down.
My wife in taking now Saphris for more than 5 month (10 mg/day) and before that, she was on Risperdal, but still, some fixed ideas don’t go away. Sometimes I ask myself how is it possible? I know it is a long process to feel well, but I expected already to notice some improvement, and I know I have to keep trying she takes its meds as prescribed and hopping she gets better and smile again.
Hi Randye!
Sure, feel free to share any information.
Yah, that is too bad he won't try it. When I got my first injection of Haldol DEC I was in the hospital, very psychotic, and didn't have a choice about whether or not to get the injection. I actually thought they were giving me a lethal injection at the time. I can totally see how someone might be either psychotically afraid of injections or just regularly afraid. I got it in the arm the first time, but I recommend getting it in the hip/butt area. It doesn't hurt there. I think that I was pretty much able to understand why I needed the injection after the first dose and then I wasn't afraid of it anymore! It cleared up my thinking a LOT! Well, I'm sorry Ben won't try it. If there is anything I can do to help, please let me know!
:) kristin
I'm curious to what the locked box comes into play with med noncompliance?
Hi Wendy ,
In our case, Ben has access to his meds, and one of them is in a liquid suspension form, which he prefers over tablets. His recent near-relapse, we believe, may have been because he discovered he could dilute this liquid and it would look relatively unchanged. Or - if we really stretch - perhaps it was not prepared properly by the pharmacist (as I said, that would be a stretch).
So, to prevent access to this medication, we locked the new batch in a cashbox with combination, so Ben has no access to it. And now his med levels are back where they belong.
We do what we must do!
Thanks,
Randye
Hi! I don't know your whole situation or anything, so please take this with a grain of salt, but have you thought about having Ben on an injectable antipsychotic? They literally saved my life. I would often go off meds and end up psychotic. I've been pretty much stable now for 13 years due in large part to taking injectable antipsychotic medication. I was getting the injectable Haldol, but I recently switched to injectable Abilify which is called Abilify Maintena. I seriously encourage anyone with schizophrenia to consider the injectable meds. They work sooooo well! Of course, each person reacts differently to different meds, so you'd need to consult a doctor...maybe try out the oral before going to the injectables or something. It can literally mean the difference between life and death.
Hi Kristin, and thanks for your suggestion. How I wish Ben would be willing to try an injectable! I am thrilled to hear how well it's working for you, and hold hope that someday Ben might open his mind to the idea. I am familiar with maintena and I keep that thought in the back of my mind for the future.
May I pass your feedback on to the folks who make maintena? They love to hear feedback!
Congrats and thanks so much for writing,
Randye
Emily. It is not as simple as that! if you have a physical condition which schizophrenia and allied disorders are, why would you try and come off meds.If you had diabetes type one you would appreciate that it would be unwise to stop taking insulin. Having a serious mental illness should be accepted as a no fault physical condition and your long term goals should not be concentrated on going off meds. Maybe in the future there will be better meds. In addition, the illnesses will no doubt be understood better and this will lead to better treatments. Patricia Forsdyke.
Coming off of meds cold turkey drastically increases the chance of relapse. I wonder if there is a way to work with his doctor to taper him down extremely slowly, if he really wants off his meds. Some studies are showing better long term functional outcomes for people who stop taking antipsychotic medication- however the benefits are long term. And you do have to get through the short term to get to the long term. The antipsychotics do help a lot with symptoms in the short term, I just just think that the brain adapts over time, and they help less and less the longer you are on them. That said, I am still taking Zyprexa. Because I have to get through my short term to get to my long term.