Managing the self-sabotaging behaviors that make life with Dissociative Identity Disorder so difficult doesn't mean getting rid of them. It means learning to live with them; recognizing and investing in the opportunities for growth inherent in self-sabotage. For me, that requires (1) acceptance of those behaviors, no matter how repugnant, (2) honest communication devoid of the power struggle that characterizes instinctual responses to self-sabotage, and (3) welcoming compromises that allow me to keep moving. When I discovered an alter was blocking internal communication, I was surprised to learn that all three of those things are possible. But it was the compromise that amazed me the most, and ultimately changed my life.
Support for DID
I define self-sabotaging behaviors within Dissociative Identity Disorder as any thought, feeling, or action by any member of the system that actively impedes the intentions and goals of any other member of the system. Self-sabotage, by my definition, is a regular part of life with DID. And what most of us do when an alter disrupts our lives in some way is attempt to change the disruptive behavior. It makes sense, but it's counter-productive. Before you know it, you're entrenched in a power struggle that ultimately solves nothing. Without even realizing it, I engaged in a power struggle for years with an alter who effectively blocked all internal communication. Once I became aware of the situation, I stopped trying to change it. I now believe acceptance is the first step in managing self-sabotaging behaviors. And communication, I think, is the second.
Self-sabotage is hard for anyone to deal with. But I think managing self-sabotaging behaviors when you have Dissociative Identity Disorder is more difficult. So when I say that I think doing so is a matter of acceptance, communication, and compromise, I don't mean to over-simplify the monumental challenge that it is. Accepting things that directly impact your life in negative, destructive ways is frightening to say the least. But the most life changing negotiation with an alter I've ever had wouldn't have happened if I hadn't done exactly that.
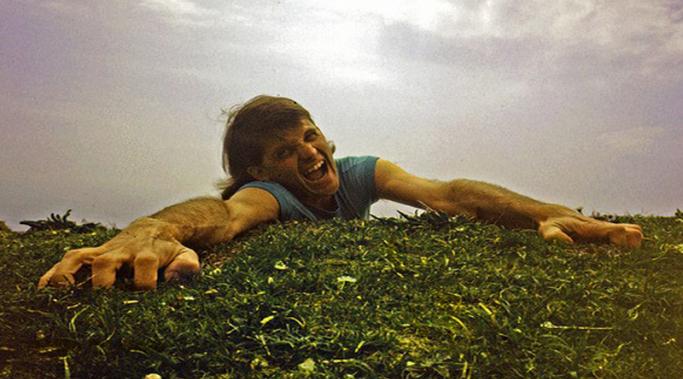
If you have dissociative identity disorder, dissociation is your primary coping mechanism. As such, it's both adaptive and maladaptive. It allows you to continue functioning despite overwhelming stress. But dissociation is also what prevents you from recognizing that you've fallen off a cliff until you hit the ground. The idea behind taking stock of mental health warning signs is to notice your free fall a little sooner. Ideally, you'd eventually have the awareness to see the edge of the cliff from a distance and avoid it altogether.
Living with dissociative identity disorder (DID) presents unique difficulties, whether you're the one that has it or the person who loves the one living with it. I can only imagine how frustrating, confusing, even painful it must sometimes be to have a partner with DID.
I've witnessed how challenging it often is for my own partner and, if some of the comments I've received here at Dissociative Living are in any way representative, her experience is typical. But it's also largely ignored. Partners of people with DID don't get that much support or encouragement, primarily because only those who've been there can truly understand (Caregiver Stress and Compassion Fatigue).
If you have Dissociative Identity Disorder, recognizing when you're on a downward spiral may be incredibly difficult. Dissociation separates us from our thoughts, feelings, and experiences and makes maintaining awareness of our very realities a monumental challenge. My hope is that by taking stock of my mental health warning signs, I can increase my chances of noticing the next decline in functioning at its inception, rather than coming out of a dissociative fog six months in and wondering what happened to my life.
Near the bottom of the HealthyPlace homepage there's an audio widget, bordered in orange with the header Share Your Mental Health Experience. If you have a spare three minutes, please play the clip titled "I Hear A Voice in My Head" and listen to one woman poignantly illustrate why I write about Dissociative Identity Disorder. This woman, like so many others, is struggling in isolation with something she doesn't understand. "People act like it's nothing," she says. No matter the condition, there will always be people who act like it's nothing. Talking about mental illness, publicly and honestly, is the only way I know to ease that kind of invalidation.
I wrote the series, Diary of a Newly Diagnosed Dissociative, because I know I'm not the only one who has wrestled in turmoil over their Dissociative Identity Disorder diagnosis. I want those who are struggling to know that, within the context of DID, their experiences aren't as unusual as they probably feel. But knowing you're not alone, while helpful, won't ease the struggle too much if there's no end in sight. I can tell you, though, that making peace with this diagnosis is an attainable goal. I did it. These three things are what made it possible.
Lately I've a greater need for Dissociative Identity Disorder support and community. But like most people with DID, I have serious trust issues. I'm far more comfortable on the fringes of any given group where I have a clearer view of the dynamics and can maintain a safe distance. Still, I'm a human being wrestling with tough stuff. I need understanding and fellowship - something many with DID find sporadically, if at all. It's important, therefore, to get the most out of whatever support we're given.
In an email conversation I had last week with someone who also has Dissociative Identity Disorder, the issue of hospitalization came up. I was impressed by this person's pro-active perspective. He appeared to accept the fact that inpatient stays are sometimes a part of the recovery process. Historically, my attitude has been much different. But I've decided his forward-thinking approach is healthier.