Rozerem: Insomnia Medicine (Full Prescribing Information)
Brand Name: Rozerem
Generic Name: Ramelteon
Ramelteon is a sedative, also called hipnotic drug that is available as Rozarem, used to treat insomnia by helping regulate "sleep-wake cycles". Usage, dosage, side effects.
Indications and Usage
Dosage and Administration
Dosage Forms and Strengths
Contraindications
Warnings and Precautions
Adverse Reactions
Drug Interactions
Use in Specific Populations
Drug Abuse and Dependence
Overdose
Description
Clinical Pharmacology
Nonclinical Toxicology
Clinical Studies
How Supplied
Rozerem patient information sheet (in plain English)
Indications and Usage
ROZEREM is indicated for the treatment of insomnia characterized by difficulty with sleep onset.
The clinical trials performed in support of efficacy were up to 6 months in duration. The final formal assessments of sleep latency were performed after 2 days of treatment during the crossover study (elderly only), at 5 weeks in the 6-week studies (adults and elderly), and at the end of the 6-month study (adults and elderly) (see Clinical Studies).
Dosage and Administration
Dosage in Adults
The recommended dose of ROZEREM is 8 mg taken within 30 minutes of going to bed. It is recommended that ROZEREM not be taken with or immediately after a high-fat meal.
The total ROZEREM dose should not exceed 8 mg per day.
Dosing in Patients with Hepatic Impairment
ROZEREM is not recommended in patients with severe hepatic impairment. ROZEREM should be used with caution in patients with moderate hepatic impairment (see Warnings and Precautions, Clinical Pharmacology).
Administration with Other Medications
ROZEREM should not be used in combination with fluvoxamine. ROZEREM should be used with caution in patients taking other CYP1A2 inhibiting drugs (see Drug Interactions, Clinical Pharmacology).
Dosage Forms And Strengths
ROZEREM is available in an 8 mg strength tablet for oral administration.
ROZEREM 8 mg tablets are round, pale orange-yellow, film-coated, with "TAK" and "RAM-8" printed on one side.
Contraindications
Patients who develop angioedema after treatment with ROZEREM should not be rechallenged with the drug.
Patients should not take ROZEREM in conjunction with fluvoxamine (Luvox) (see Drug Interactions).
WARNINGS AND PRECAUTIONS
Severe Anaphylactic and Anaphylactoid Reactions
Rare cases of angioedema involving the tongue, glottis or larynx have been reported in patients after taking the first or subsequent doses of ROZEREM. Some patients have had additional symptoms such as dyspnea, throat closing, or nausea and vomiting that suggest anaphylaxis. Some patients have required medical therapy in the emergency department. If angioedema involves the tongue, glottis or larynx, airway obstruction may occur and be fatal. Patients who develop angioedema after treatment with ROZEREM should not be rechallenged with the drug.
Need to Evaluate for Co-morbid Diagnoses
 Since sleep disturbances may be the presenting manifestation of a physical and/or psychiatric disorder, symptomatic treatment of insomnia should be initiated only after a careful evaluation of the patient. The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. Worsening of insomnia, or the emergence of new cognitive or behavioral abnormalities, may be the result of an unrecognized underlying psychiatric or physical disorder and requires further evaluation of the patient. Exacerbation of insomnia and emergence of cognitive and behavioral abnormalities were seen with ROZEREM during the clinical development program.
Since sleep disturbances may be the presenting manifestation of a physical and/or psychiatric disorder, symptomatic treatment of insomnia should be initiated only after a careful evaluation of the patient. The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. Worsening of insomnia, or the emergence of new cognitive or behavioral abnormalities, may be the result of an unrecognized underlying psychiatric or physical disorder and requires further evaluation of the patient. Exacerbation of insomnia and emergence of cognitive and behavioral abnormalities were seen with ROZEREM during the clinical development program.
Abnormal Thinking and Behavioral Changes
A variety of cognitive and behavior changes have been reported to occur in association with the use of hypnotics. In primarily depressed patients, worsening of depression (including suicidal ideation and completed suicides) has been reported in association with the use of hypnotics.
Hallucinations, as well as behavioral changes such as bizarre behavior, agitation and mania have been reported with ROZEREM use. Amnesia, anxiety and other neuro-psychiatric symptoms may also occur unpredictably.
Complex behaviors such as "sleep-driving" (i.e., driving while not fully awake after ingestion of a hypnotic) and other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex), with amnesia for the event, have been reported in association with hypnotic use. The use of alcohol and other CNS depressants may increase the risk of such behaviors. These events can occur in hypnotic-naive as well as in hypnotic-experienced persons. Complex behaviors have been reported with the use of ROZEREM. Discontinuation of ROZEREM should be strongly considered for patients who report any complex sleep behavior.
CNS Effects
Patients should avoid engaging in hazardous activities that require concentration (such as operating a motor vehicle or heavy machinery) after taking ROZEREM.
After taking ROZEREM, patients should confine their activities to those necessary to prepare for bed.
Patients should be advised not to consume alcohol in combination with ROZEREM as alcohol and ROZEREM may have additive effects when used in conjunction.
Reproductive Effects
Use in Adolescents and Children
ROZEREM has been associated with an effect on reproductive hormones in adults, e.g., decreased testosterone levels and increased prolactin levels. It is not known what effect chronic or even chronic intermittent use of ROZEREM may have on the reproductive axis in developing humans (see Clinical Trials).
Use in Patients with Concomitant Illness
ROZEREM has not been studied in subjects with severe sleep apnea and is not recommended for use in this population (see Use in Specific Populations).
ROZEREM should not be used by patients with severe hepatic impairment (see Clinical Pharmacology).
Laboratory Tests
Monitoring
No standard monitoring is required.
For patients presenting with unexplained amenorrhea, galactorrhea, decreased libido, or problems with fertility, assessment of prolactin levels and testosterone levels should be considered as appropriate.
Interference with laboratory tests
ROZEREM is not known to interfere with commonly used clinical laboratory tests. In addition, in vitro data indicate that ramelteon does not cause false-positive results for benzodiazepines, opiates, barbiturates, cocaine, cannabinoids, or amphetamines in two standard urine drug screening methods in vitro.
Adverse Reactions
Severe Anaphylactic and Anaphylactoid Reactions
Rare cases of angioedema involving the tongue, glottis or larynx have been reported in patients after taking the first or subsequent doses of ROZEREM. Some patients have had additional symptoms such as dyspnea, throat closing, or nausea and vomiting that suggest anaphylaxis. Some patients have required medical therapy in the emergency department. If angioedema involves the tongue, glottis or larynx, airway obstruction may occur and be fatal. Patients who develop angioedema after treatment with ROZEREM should not be rechallenged with the drug.
Need to Evaluate for Co-morbid Diagnoses
Since sleep disturbances may be the presenting manifestation of a physical and/or psychiatric disorder, symptomatic treatment of insomnia should be initiated only after a careful evaluation of the patient. The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. Worsening of insomnia, or the emergence of new cognitive or behavioral abnormalities, may be the result of an unrecognized underlying psychiatric or physical disorder and requires further evaluation of the patient. Exacerbation of insomnia and emergence of cognitive and behavioral abnormalities were seen with ROZEREM during the clinical development program.
Abnormal Thinking and Behavioral Changes
A variety of cognitive and behavior changes have been reported to occur in association with the use of hypnotics. In primarily depressed patients, worsening of depression (including suicidal ideation and completed suicides) has been reported in association with the use of hypnotics.
Hallucinations, as well as behavioral changes such as bizarre behavior, agitation and mania have been reported with ROZEREM use. Amnesia, anxiety and other neuro-psychiatric symptoms may also occur unpredictably.
Complex behaviors such as "sleep-driving" (i.e., driving while not fully awake after ingestion of a hypnotic) and other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex), with amnesia for the event, have been reported in association with hypnotic use. The use of alcohol and other CNS depressants may increase the risk of such behaviors. These events can occur in hypnotic-naive as well as in hypnotic-experienced persons. Complex behaviors have been reported with the use of ROZEREM. Discontinuation of ROZEREM should be strongly considered for patients who report any complex sleep behavior.
CNS Effects
Patients should avoid engaging in hazardous activities that require concentration (such as operating a motor vehicle or heavy machinery) after taking ROZEREM.
After taking ROZEREM, patients should confine their activities to those necessary to prepare for bed.
Patients should be advised not to consume alcohol in combination with ROZEREM as alcohol and ROZEREM may have additive effects when used in conjunction.
Reproductive Effects
Use in Adolescents and Children
ROZEREM has been associated with an effect on reproductive hormones in adults, e.g., decreased testosterone levels and increased prolactin levels. It is not known what effect chronic or even chronic intermittent use of ROZEREM may have on the reproductive axis in developing humans (see Clinical Trials).
Use in Patients with Concomitant Illness
ROZEREM has not been studied in subjects with severe sleep apnea and is not recommended for use in this population (see Use in Specific Populations).
ROZEREM should not be used by patients with severe hepatic impairment (see Clinical Pharmacology).
Laboratory Tests
Monitoring
No standard monitoring is required.
For patients presenting with unexplained amenorrhea, galactorrhea, decreased libido, or problems with fertility, assessment of prolactin levels and testosterone levels should be considered as appropriate.
Interference with laboratory tests
ROZEREM is not known to interfere with commonly used clinical laboratory tests. In addition, in vitro data indicate that ramelteon does not cause false-positive results for benzodiazepines, opiates, barbiturates, cocaine, cannabinoids, or amphetamines in two standard urine drug screening methods in vitro.
| MedDRA Preferred Term | Placebo (n=1456) |
Ramelteon 8 mg (n=1405) |
| Somnolence | 2% | 3% |
| Fatigue | 2% | 3% |
| Dizziness | 3% | 4% |
| Nausea | 2% | 3% |
| Insomnia exacerbated | 2% | 3% |
Drug Interactions
Effects of Other Drugs on ROZEREM
Fluvoxamine (strong CYP1A2 inhibitor): AUC0-inf for ramelteon increased approximately 190-fold, and the Cmax increased approximately 70-fold upon coadministration of fluvoxamine and ROZEREM, compared to ROZEREM administered alone. ROZEREM should not be used in combination with fluvoxamine (see Contraindications, Clinical Pharmacology). Other less strong CYP1A2 inhibitors have not been adequately studied. ROZEREM should be administered with caution to patients taking less strong CYP1A2 inhibitors.
Rifampin (strong CYP enzyme inducer): Administration of multiple doses of rifampin once daily for 11 days resulted in a mean decrease of approximately 80% (40% to 90%) in total exposure to ramelteon. Efficacy may be reduced when ROZEREM is used in combination with strong CYP enzyme inducers such as rifampin (see Clinical Pharmacology).
Ketoconazole (strong CYP3A4 inhibitor): The AUC0-inf and Cmax of ramelteon increased by approximately 84% and 36% upon coadministration of ketoconazole with ROZEREM. ROZEREM should be administered with caution in subjects taking strong CYP3A4 inhibitors such as ketoconazole (see Clinical Pharmacology).
Fluconazole (strong CYP2C9 inhibitor): The AUC0-inf and Cmax of ramelteon was increased by approximately 150% when ROZEREM was coadministered with fluconazole. ROZEREM should be administered with caution in subjects taking strong CYP2C9 inhibitors such as fluconazole (see Clinical Pharmacology).
Effect of Alcohol on ROZEREM
Alcohol by itself impairs performance and can cause sleepiness. Since the intended effect of ROZEREM is to promote sleep, patients should be cautioned not to consume alcohol when using ROZEREM (see Clinical Pharmacology). Use of the products in combination may have an additive effect.
Drug/Laboratory Test Interactions
ROZEREM is not known to interfere with commonly used clinical laboratory tests. In addition, in vitro data indicate that ramelteon does not cause false-positive results for benzodiazepines, opiates, barbiturates, cocaine, cannabinoids, or amphetamines in two standard urine drug screening methods in vitro.
Use In Specific Populations
Pregnancy
Pregnancy Category C
In animal studies, ramelteon produced evidence of developmental toxicity, including teratogenic effects, in rats at doses much greater than the recommended human dose (RHD) of 8 mg/day. There are no adequate and well-controlled studies in pregnant women. ROZEREM should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Oral administration of ramelteon (10, 40, 150 or 600 mg/kg/day) to pregnant rats during the period of organogenesis was associated with increased incidences of fetal structural abnormalities (malformations and variations) at doses greater than 40 mg/kg/day. The no-effect dose is approximately 50 times the RHD on a body surface area (mg/m2) basis. Treatment of pregnant rabbits during the period of organogenesis produced no evidence of embryo-fetal toxicity at oral doses of up to 300 mg/kg/day (or up to 720 times the RHD on a mg/m2 basis).
When rats were orally administered ramelteon (30, 100, or 300 mg/kg/day) throughout gestation and lactation, growth retardation, developmental delay, and behavioral changes were observed in the offspring at doses greater than 30 mg/kg/day. The no-effect dose is 36 times the RHD on a mg/m2 basis. Increased incidences of malformation and death among offspring were seen at the highest dose.
Labor and delivery
The potential effects of ROZEREM on the duration of labor and/or delivery, for either the mother or the fetus, have not been studied. ROZEREM has no established use in labor and delivery.
Nursing Mothers
It is not known whether ramelteon is secreted into human milk; however ramelteon is secreted into the milk of lactating rats. Because many drugs are excreted into human milk, caution should be exercised when administered to a nursing woman.
Pediatric Use
Safety and effectiveness of ROZEREM in pediatric patients have not been established. Further study is needed prior to determining that this product may be used safely in pre-pubescent and pubescent patients.
Geriatric Use
A total of 654 subjects in double-blind, placebo-controlled, efficacy trials who received ROZEREM were at least 65 years of age; of these, 199 were 75 years of age or older. No overall differences in safety or efficacy were observed between elderly and younger adult subjects.
A double-blind, randomized, placebo-controlled study in elderly subjects with insomnia (n=33) evaluated the effect of a single dose of ROZEREM on balance, mobility, and memory functions after middle of the night awakening. There is no information on the effect of multiple dosing. Night time dosing of ROZEREM 8 mg did not impair middle of the night balance, mobility, or memory functions relative to placebo. The effects on night balance in the elderly cannot be definitively known from this study.
Chronic Obstructive Pulmonary Disease
The respiratory depressant effect of ROZEREM was evaluated in a crossover design study of subjects (n=26) with mild to moderate COPD after administering a single 16 mg dose or placebo, and in a separate study (n=25), the effects of ROZEREM on respiratory parameters were evaluated after administering an 8 mg dose or placebo in a crossover design to patients with moderate to severe COPD, defined as patients who had forced expiratory volume at one second (FEV1)/forced vital capacity ratio of <70%, and a FEV1 <80% of predicted with <12% reversibility to albuterol. Treatment with a single dose of ROZEREM has no demonstrable respiratory depressant effects in subjects with mild to severe COPD, as measured by arterial O2 saturation (SaO2). There is no available information on the respiratory effects of multiple doses of ROZEREM in patients with COPD. The respiratory depressant effects in patients with COPD cannot be definitively known from this study.
Sleep Apnea
The effects of ROZEREM were evaluated after administering a 16 mg dose or placebo in a crossover design to subjects (n=26) with mild to moderate obstructive sleep apnea. Treatment with ROZEREM 16 mg for one night showed no difference compared with placebo on the Apnea/Hypopnea Index (the primary outcome variable), apnea index, hypopnea index, central apnea index, mixed apnea index, and obstructive apnea index. Treatment with a single dose of ROZEREM does not exacerbate mild to moderate obstructive sleep apnea. There is no available information on the respiratory effects of multiple doses of ROZEREM in patients with sleep apnea. The effects on exacerbation in patients with mild to moderate sleep apnea cannot be definitively known from this study.
ROZEREM has not been studied in subjects with severe obstructive sleep apnea; use of ROZEREM is not recommended in such patients.
Hepatic Impairment
Exposure to ROZEREM was increased by 4-fold in subjects with mild hepatic impairment and by more than 10-fold in subjects with moderate hepatic impairment. ROZEREM should be used with caution in patients with moderate hepatic impairment (see Clinical Pharmacology). ROZEREM is not recommended in patients with severe hepatic impairment.
Renal Impairment
No effects on Cmax and AUC0-t of parent drug or M-II were seen. No adjustment of ROZEREM dosage is required in patients with renal impairment (see Clinical Pharmacology).
Drug Abuse And Dependence
ROZEREM is not a controlled substance.
Discontinuation of ramelteon in animals or in humans after chronic administration did not produce withdrawal signs. Ramelteon does not appear to produce physical dependence.
Human Data: A laboratory abuse potential study was performed with ROZEREM (see Clinical Studies).
Animal Data: Ramelteon did not produce any signals from animal behavioral studies indicating that the drug produces rewarding effects. Monkeys did not self-administer ramelteon and the drug did not induce a conditioned place preference in rats. There was no generalization between ramelteon and midazolam. Ramelteon did not affect rotorod performance, an indicator of disruption of motor function, and it did not potentiate the ability of diazepam to interfere with rotorod performance.
Overdose
General symptomatic and supportive measures should be used, along with immediate gastric lavage where appropriate. Intravenous fluids should be administered as needed. As in all cases of drug overdose, respiration, pulse, blood pressure, and other appropriate vital signs should be monitored, and general supportive measures employed.
Hemodialysis does not effectively reduce exposure to ROZEREM. Therefore, the use of dialysis in the treatment of overdosage is not appropriate.
Poison Control Center: As with the management of all overdosage, the possibility of multiple drug ingestion should be considered. Contact a poison control center for current information on the management of overdosage.
Description
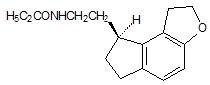
ROZEREM (ramelteon) is an orally active hypnotic chemically designated as (S)-N-[2-(1,6,7,8-tetrahydro-2H-indeno-[5,4-b]furan-8-yl)ethyl]propionamide and containing one chiral center. The compound is produced as the (S)-enantiomer, with an empirical formula of C16H21NO2, molecular weight of 259.34, and the following chemical structure:
Ramelteon is freely soluble in organic solvents, such as methanol, ethanol, and dimethyl sulfoxide; soluble in 1-octanol and acetonitrile; and very slightly soluble in water and in aqueous buffers from pH 3 to pH 11.
Each ROZEREM tablet includes the following inactive ingredients: lactose monohydrate, starch, hydroxypropyl cellulose, magnesium stearate, hypromellose, copovidone, titanium dioxide, yellow ferric oxide, polyethylene glycol 8000, and ink containing shellac and synthetic iron oxide black.
Clinical Pharmacology
Mechanism of Action
ROZEREM (ramelteon) is a melatonin receptor agonist with both high affinity for melatonin MT1 and MT2 receptors and selectivity over the MT3 receptor. Ramelteon demonstrates full agonist activity in vitro in cells expressing human MT1 or MT2 receptors.
The activity of ramelteon at the MT1 and MT2 receptors is believed to contribute to its sleep-promoting properties, as these receptors, acted upon by endogenous melatonin, are thought to be involved in the maintenance of the circadian rhythm underlying the normal sleep-wake cycle.
Ramelteon has no appreciable affinity for the GABA receptor complex or for receptors that bind neuropeptides, cytokines, serotonin, dopamine, noradrenaline, acetylcholine, and opiates. Ramelteon also does not interfere with the activity of a number of selected enzymes in a standard panel.
The major metabolite of ramelteon, M-II, is active and has approximately one tenth and one fifth the binding affinity of the parent molecule for the human MT1 and MT2 receptors, respectively, and is 17- to 25-fold less potent than ramelteon in in vitro functional assays. Although the potency of M-II at MT1 and MT2 receptors is lower than the parent drug, M-II circulates at higher concentrations than the parent producing 20- to 100-fold greater mean systemic exposure when compared to ramelteon. M-II has weak affinity for the serotonin 5-HT2B receptor, but no appreciable affinity for other receptors or enzymes. Similar to ramelteon, M-II does not interfere with the activity of a number of endogenous enzymes.
All other known metabolites of ramelteon are inactive.
Pharmacokinetics
The pharmacokinetic profile of ROZEREM has been evaluated in healthy subjects as well as in subjects with hepatic or renal impairment. When administered orally to humans in doses ranging from 4 to 64 mg, ramelteon undergoes rapid, high first-pass metabolism, and exhibits linear pharmacokinetics. Maximal serum concentration (Cmax) and area under the concentration-time curve (AUC) data show substantial intersubject variability, consistent with the high first-pass effect; the coefficient of variation for these values is approximately 100%. Several metabolites have been identified in human serum and urine.
Absorption
Ramelteon is absorbed rapidly, with median peak concentrations occurring at approximately 0.75 hour (range, 0.5 to 1.5 hours) after fasted oral administration. Although the total absorption of ramelteon is at least 84%, the absolute oral bioavailability is only 1.8% due to extensive first-pass metabolism.
Distribution
In vitro protein binding of ramelteon is approximately 82% in human serum, independent of concentration. Binding to albumin accounts for most of that binding, since 70% of the drug is bound in human serum albumin. Ramelteon is not distributed selectively to red blood cells.
Ramelteon has a mean volume of distribution after intravenous administration of 73.6 L, suggesting substantial tissue distribution.
Metabolism
Metabolism of ramelteon consists primarily of oxidation to hydroxyl and carbonyl derivatives, with secondary metabolism producing glucuronide conjugates. CYP1A2 is the major isozyme involved in the hepatic metabolism of ramelteon; the CYP2C subfamily and CYP3A4 isozymes are also involved to a minor degree.
The rank order of the principal metabolites by prevalence in human serum is M-II, M-IV, M-I, and M-III. These metabolites are formed rapidly and exhibit a monophasic decline and rapid elimination. The overall mean systemic exposure of M-II is approximately 20- to 100-fold higher than parent drug.
Elimination
Following oral administration of radiolabeled ramelteon, 84% of total radioactivity was excreted in urine and approximately 4% in feces, resulting in a mean recovery of 88%. Less than 0.1% of the dose was excreted in urine and feces as the parent compound. Elimination was essentially complete by 96 hours post-dose.
Repeated once daily dosing with ROZEREM does not result in significant accumulation owing to the short elimination half-life of ramelteon (on average, approximately 1- 2.6 hours).
The half-life of M-II is 2 to 5 hours and independent of dose. Serum concentrations of the parent drug and its metabolites in humans are at or below the lower limits of quantitation within 24 hours.
Effect of Food
When administered with a high-fat meal, the AUC0-inf for a single 16 mg dose of ROZEREM was 31% higher and the Cmax was 22% lower than when given in a fasted state. Median Tmax was delayed by approximately 45 minutes when ROZEREM was administered with food. Effects of food on the AUC values for M-II were similar. It is therefore recommended that ROZEREM not be taken with or immediately after a high-fat meal (see Dosage and Administration).
Pharmacokinetics in Special Populations
Age: In a group of 24 elderly subjects aged 63 to 79 years administered a single ROZEREM 16 mg dose, the mean Cmax and AUC0-inf values were 11.6 ng/mL (SD, 13.8) and 18.7 ng·hr/mL (SD, 19.4), respectively. The elimination half-life was 2.6 hours (SD, 1.1). Compared with younger adults, the total exposure (AUC0-inf) and Cmax of ramelteon were 97% and 86% higher, respectively, in elderly subjects. The AUC0-inf and Cmax of M-II were increased by 30% and 13%, respectively, in elderly subjects.
Gender: There are no clinically meaningful gender-related differences in the pharmacokinetics of ROZEREM or its metabolites.
Hepatic Impairment: Exposure to ROZEREM was increased almost 4-fold in subjects with mild hepatic impairment after 7 days of dosing with 16 mg/day; exposure was further increased (more than 10-fold) in subjects with moderate hepatic impairment. Exposure to M-II was only marginally increased in mildly and moderately impaired subjects relative to healthy matched controls. The pharmacokinetics of ROZEREM have not been evaluated in subjects with severe hepatic impairment (Child-Pugh Class C). ROZEREM should be used with caution in patients with moderate hepatic impairment (see Warnings and Precautions).
Renal Impairment: The pharmacokinetic characteristics of ROZEREM were studied after administering a 16 mg dose to subjects with mild, moderate, or severe renal impairment based on pre-dose creatinine clearance (53 to 95, 35 to 49, or 15 to 30 mL/min/1.73 m2, respectively), and in subjects who required chronic hemodialysis. Wide intersubject variability was seen in ROZEREM exposure parameters. However, no effects on Cmax or AUC0-t of parent drug or M-II were seen in any of the treatment groups; the incidence of adverse events was similar across groups. These results are consistent with the negligible renal clearance of ramelteon, which is principally eliminated via hepatic metabolism. No adjustment of ROZEREM dosage is required in patients with renal impairment, including patients with severe renal impairment (creatinine clearance of ≤ 30 mL/min/1.73 m2) and patients who require chronic hemodialysis.
Drug-Drug Interactions
ROZEREM has a highly variable intersubject pharmacokinetic profile (approximately 100% coefficient of variation in Cmax and AUC). As noted above, CYP1A2 is the major isozyme involved in the metabolism of ROZEREM; the CYP2C subfamily and CYP3A4 isozymes are also involved to a minor degree.
Effects of Other Drugs on ROZEREM Metabolism
Fluvoxamine (strong CYP1A2 inhibitor): When fluvoxamine 100 mg twice daily was administered for 3 days prior to single-dose co-administration of ROZEREM 16 mg and fluvoxamine, the AUC0-inf for ramelteon increased approximately 190-fold, and the Cmax increased approximately 70-fold, compared to ROZEREM administered alone. ROZEREM should not be used in combination with fluvoxamine. Other less strong CYP1A2 inhibitors have not been adequately studied. ROZEREM should be administered with caution to patients taking less strong CYP1A2 inhibitors (see Contraindications).
Rifampin (strong CYP enzyme inducer): Administration of rifampin 600 mg once daily for 11 days resulted in a mean decrease of approximately 80% (40% to 90%) in total exposure to ramelteon and metabolite M-II, (both AUC0-inf and Cmax) after a single 32 mg dose of ROZEREM. Efficacy may be reduced when ROZEREM is used in combination with strong CYP enzyme inducers such as rifampin.
Ketoconazole (strong CYP3A4 inhibitor): The AUC0-inf and Cmax of ramelteon increased by approximately 84% and 36%, respectively, when a single 16 mg dose of ROZEREM was administered on the fourth day of ketoconazole 200 mg twice daily administration, compared to administration of ROZEREM alone. Similar increases were seen in M-II pharmacokinetic variables. ROZEREM should be administered with caution in subjects taking strong CYP3A4 inhibitors such as ketoconazole.
Fluconazole (strong CYP2C9 inhibitor): The total and peak systemic exposure (AUC0-inf and Cmax) of ramelteon after a single 16 mg dose of ROZEREM was increased by approximately 150% when administered with fluconazole. Similar increases were also seen in M-II exposure. ROZEREM should be administered with caution in subjects taking strong CYP2C9 inhibitors such as fluconazole.
Interaction studies of concomitant administration of ROZEREM with fluoxetine (CYP2D6 inhibitor), omeprazole (CYP1A2 inducer/CYP2C19 inhibitor), theophylline (CYP1A2 substrate), and dextromethorphan (CYP2D6 substrate) did not produce clinically meaningful changes in either peak or total exposures to ramelteon or the M-II metabolite.
Effects of ROZEREM on Metabolism of Other Drugs
Concomitant administration of ROZEREM with omeprazole (CYP2C19 substrate), dextromethorphan (CYP2D6 substrate), midazolam (CYP3A4 substrate), theophylline (CYP1A2 substrate), digoxin (p-glycoprotein substrate) and warfarin (CYP2C9 [S]/CYP1A2 [R] substrate) did not produce clinically meaningful changes in peak and total exposures to these drugs.
Effect of Alcohol on ROZEREM
With single-dose, daytime co-administration of ROZEREM 32 mg and alcohol (0.6 g/kg), there were no clinically meaningful or statistically significant effects on peak or total exposure to ROZEREM. However, an additive effect was seen on some measures of psychomotor performance (i.e., the Digit Symbol Substitution Test, the Psychomotor Vigilance Task Test, and a Visual Analog Scale of Sedation) at some post-dose time points. No additive effect was seen on the Delayed Word Recognition Test. Because alcohol by itself impairs performance, and the intended effect of ROZEREM is to promote sleep, patients should be cautioned not to consume alcohol when using ROZEREM.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Ramelteon was administered to mice and rats at oral doses of 0, 30, 100, 300, or 1000 mg/kg/day (mice) and 0, 15, 60, 250, or 1000 mg/kg/day (rats). Mice and rats were dosed for two years, except at the high dose (94 weeks for male and female mice and female rats). In mice, dose-related increases in the incidence of hepatic tumors (adenomas, carcinomas, hepatoblastomas) were observed in males and females. The no-effect dose for hepatic tumors in mice (30 mg/kg/day) is approximately 20 times the recommended human dose (RHD) of 8 mg/day on a body surface area (mg/m2) basis.
In rats, the incidence of hepatic adenoma and benign Leydig cell tumors of the testis was increased in males at doses ≥ 250 mg/kg/day. In females, the incidence of hepatic adenoma was increased at doses ≥ 60 mg/kg/day. The incidence of hepatic carcinoma was increased in males and female rats at 1000 mg/kg/day. The no-effect dose for tumors in rats (15 mg/kg/day) is approximately 20 times the RHD on a mg/m2 basis.
Mutagenesis
Ramelteon was not genotoxic in the in vitro bacterial reverse mutation (Ames) assay, the in vitro mouse lymphoma TK+/- assay, and in in vivo oral micronucleus assays in mouse and rat. Ramelteon was clastogenic in the in vitro chromosomal aberration assay in Chinese hamster lung cells.
Separate studies indicated that the concentration of the M-II metabolite formed in the presence of metabolic activation exceeded the concentration of ramelteon; therefore, the genotoxic potential of the M-II metabolite was also assessed in the in vitro studies.
Impairment of Fertility
When ramelteon (doses of 6 to 600 mg/kg/day) was administered orally to male and female rats prior to and during mating and early gestation, alterations in estrus cyclicity and decreased numbers of corpora lutea, implantations, and live embryos were observed at doses greater than 20 mg/kg/day. The no-effect dose is approximately 24 times the recommended human dose of 8 mg/day on a body surface area (mg/m2) basis. Oral administration of ramelteon (up to 600 mg/kg/day) to male rats had no effects on sperm quality or reproductive performance.
Clinical Studies
Controlled Clinical Trials
Chronic Insomnia
Three randomized, double-blind trials in subjects with chronic insomnia employing polysomnography (PSG) were provided as objective support of ROZEREM's effectiveness in sleep initiation.
One study enrolled younger adults (aged 18 to 64 years, inclusive) with chronic insomnia and employed a parallel design in which the subjects received a single, nightly dose of ROZEREM (8 mg or 16 mg) or matching placebo for 35 days. PSG was performed on the first two nights in each of Weeks 1, 3, and 5 of treatment. ROZEREM reduced the average latency to persistent sleep at each of the time points when compared to placebo. The 16 mg dose conferred no additional benefit for sleep initiation.
The second study employing PSG was a three-period crossover trial performed in subjects aged 65 years and older with a history of chronic insomnia. Subjects received ROZEREM (4 mg or 8 mg) or placebo and underwent PSG assessment in a sleep laboratory for two consecutive nights in each of the three study periods. Both doses of ROZEREM reduced latency to persistent sleep when compared to placebo.
The third study evaluated long term efficacy and safety in adults with chronic insomnia. Subjects received a single, nightly dose of ROZEREM 8 mg or matching placebo for 6 months. PSG was performed on the first two nights of Week 1 and Months 1, 3, 5, and 6. ROZEREM reduced sleep latency at each time point when compared to placebo. In this study, when the PSG results from nights 1 and 2 of Month 7 were compared to the results from nights 22 and 23 of Month 6, there was a statistically significant increase in LPS of 33% (9.5 minutes) in the ramelteon group. There was no increase in LPS in the placebo group when the same time periods were compared.
A randomized, double-blind, parallel group study was conducted in outpatients aged 65 years and older with chronic insomnia and employed subjective measures of efficacy (sleep diaries). Subjects received ROZEREM (4 mg or 8 mg) or placebo for 35 nights. ROZEREM reduced patient-reported sleep latency compared to placebo. A similarly designed study performed in younger adults (aged 18-64 years) using 8 mg and 16 mg of ramelteon did not replicate this finding of reduced patient-reported sleep latency compared to placebo.
While the 16 mg dose was evaluated as a potential treatment for adults, it was shown to confer no additional benefit for sleep initiation and was associated with higher incidences of fatigue, headache and next-day somnolence.
Transient Insomnia
In a randomized, double-blind, parallel-group trial using a first-night-effect model, healthy adults received placebo or ROZEREM before spending one night in a sleep laboratory and being evaluated with PSG. ROZEREM demonstrated a decrease in mean latency to persistent sleep as compared to placebo.
Studies Pertinent to Safety Concerns for Sleep-promoting Drugs
Results from Human Laboratory Abuse Liability Studies
A human laboratory abuse potential study was performed in 14 subjects with a history of sedative/hypnotic or anxiolytic drug abuse. Subjects received single oral doses of ROZEREM (16, 80, or 160 mg), triazolam (0.25, 0.50, or 0.75 mg) or placebo. All subjects received each of the 7 treatments separated by a wash-out period and underwent multiple standard tests of abuse potential. No differences in subjective responses indicative of abuse potential were found between ROZEREM and placebo at doses up to 20 times the recommended therapeutic dose. The positive control drug, triazolam, consistently showed a dose-response effect on these subjective measures, as demonstrated by the differences from placebo in peak effect and overall 24-hour effect.
Residual Pharmacological Effect in Insomnia Trials
In order to evaluate potential next-day residual effects, the following scales were used: a Memory Recall Test, a Word List Memory Test, a Visual Analog Mood and Feeling Scale, the Digit-Symbol Substitution Test, and a post-sleep questionnaire to assess alertness and ability to concentrate. There was no evidence of next-day residual effect seen after 2 nights of ramelteon use during the crossover studies.
In a 35-night, double-blind, placebo-controlled, parallel-group study in adults with chronic insomnia, measures of residual effects were performed at three time points. Overall, the magnitudes of any observed differences were small. At Week 1, patients who received 8 mg of ROZEREM had a mean VAS score (46 mm on a 100 mm scale) indicating more fatigue in comparison to patients who received placebo (42 mm). At Week 3, patients who received 8 mg of ROZEREM had a lower mean score for immediate recall (7.5 out of 16 words) compared to patients who received placebo (8.2 words); and the patients treated with ROZEREM had a mean VAS score indicating more sluggishness (27 mm on a 100 mm VAS) in comparison to the placebo-treated patients (22 mm). Patients who received ROZEREM did not have next-morning residual effects that were different from placebo at Week 5.
Rebound Insomnia/Withdrawal
Potential rebound insomnia and withdrawal effects were assessed in four studies in which subjects received ROZEREM or placebo for up to 6 months; 3 were 35-day studies, one was a 6 month study. These studies included a total of 2533 subjects, of whom 854 were elderly.
Tyrer Benzodiazepine Withdrawal Symptom Questionnaire (BWSQ): The BWSQ is a self-report questionnaire that solicits specific information on 20 symptoms commonly experienced during withdrawal from benzodiazepine receptor agonists; ROZEREM is not a benzodiazepine receptor agonist.
In two of the three 35-day insomnia studies, the questionnaire was administered one week after completion of treatment; in the third study, the questionnaire was administered on Days 1 and 2 after completion. In all three of the 35-day studies, subjects receiving ROZEREM 4 mg, 8 mg, or 16 mg daily reported BWSQ scores similar to those of subjects receiving placebo.
In the 6 month study, there was no evidence of withdrawal from the 8 mg dose as measured by the BWSQ.
Rebound Insomnia: Rebound insomnia was assessed in the 35-day studies by measuring sleep latency after abrupt treatment discontinuation. One of these studies employed PSG in younger adult subjects receiving ROZEREM 8 mg or 16 mg; the other two studies employed subjective measures of sleep-onset insomnia in elderly subjects receiving ROZEREM 4 mg or 8 mg, and in younger adult subjects receiving ROZEREM 8 mg or 16 mg. There was no evidence that ROZEREM caused rebound insomnia during the post-treatment period.
Studies to Evaluate Effects on Endocrine Function
Two controlled studies evaluated the effects of ROZEREM on endocrine function.
In the first trial, ROZEREM 16 mg once daily or placebo was administered to 99 healthy volunteer subjects for 4 weeks. This study evaluated the thyroid axis, adrenal axis and reproductive axis. No clinically significant endocrinopathies were demonstrated in this study. However, the study was limited in its ability to detect such abnormalities due to its limited duration.
In the second trial, ROZEREM 16 mg once daily or placebo was administered to 122 subjects with chronic insomnia for 6 months. This study evaluated the thyroid axis, adrenal axis and reproductive axis. There were no significant abnormalities seen in either the thyroid or the adrenal axes. Abnormalities were, however, noted within the reproductive axis. Overall, the mean serum prolactin level change from baseline was 4.9 μg/L (34% increase) for women in the ROZEREM group compared with −0.6 μg/L (4% decrease) for women in the placebo group (p=0.003). No differences between active- and placebo-treated groups occurred among men. Thirty-two percent of all patients who were treated with ramelteon in this study (women and men) had prolactin levels that increased from normal baseline levels compared to 19% of patients who were treated with placebo. Subject-reported menstrual patterns were similar between the two treatment groups.
In a 12-month, open-label study in adult and elderly patients, there were two patients who were noted to have abnormal morning cortisol levels, and subsequent abnormal ACTH stimulation tests. A 29-year-old female patient was diagnosed with a prolactinoma. The relationship of these events to ROZEREM therapy is not clear.
How Supplied/Storage and Handling
ROZEREM is available as round, pale orange-yellow, film-coated, 8 mg tablets, with "TAK" and "RAM-8" printed on one side, in the following quantities:
NDC 64764-805-30 Bottles of 30
NDC 64764-805-10 Bottles of 100
NDC 64764-805-50 Bottles of 500
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) (see USP controlled room temperature). Keep container tightly closed and protected from moisture and humidity.
last updated 08/08
Rozerem patient information sheet (in plain English)
Detailed Info on Signs, Symptoms, Causes, Treatments of Sleep Disorders
The information in this monograph is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects. This information is generalized and is not intended as specific medical advice. If you have questions about the medicines you are taking or would like more information, check with your doctor, pharmacist, or nurse.
back to:
~ all articles on sleeping disorders
APA Reference
Staff, H.
(2019, August 31). Rozerem: Insomnia Medicine (Full Prescribing Information), HealthyPlace. Retrieved
on 2026, March 6 from https://www.healthyplace.com/other-info/sleep-disorders/rozerem-insomnia-medicine-full-prescribing-information