Symbyax Patient Information
Find out why Symbyax is prescribed, side effects of Symbyax, Symbyax warnings, effects of Symbyax during pregnancy, more - in plain English.
Symbyax is a combination of Zyprexa and Prozac.
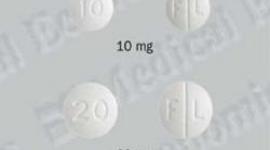
SYMBYAX® (SIM-bee-ax)
(olanzapine and fluoxetine HCl capsules)
Read the Patient Information that comes with SYMBYAX before you start using it and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or treatment. It is important to stay under a doctor s care while taking SYMBYAX. Do not change or stop treatment without first talking with your doctor. Talk to your doctor or pharmacist if you have any questions about
SYMBYAX.
Full Symbyax Prescribing Information
What is SYMBYAX?
SYMBYAX is a prescription medicine used to treat adults who have depression with bipolar disorder. SYMBYAX contains two medicines, olanzapine and fluoxetine hydrochloride.
Olanzapine is also the active ingredient in Zyprexa® and Zyprexa Zydis®. Fluoxetine hydrochloride is also the active ingredient in Prozac®, Prozac Weekly , and Sarafem®. SYMBYAX has not been studied in children.
What is bipolar disorder?
Bipolar disorder, once called manic-depressive illness, is a brain disorder that causes unusual changes in a person s mood, energy level, and ability to function. Bipolar disorder is a long-term illness that can be treated with medicines, but it usually requires life-long treatment.
Who should not take SYMBYAX?
Do not take SYMBYAX if you are:
- Taking a medicine known as a monoamine oxidase inhibitor (MAOI) or have stopped taking a MAOI within the last 2 weeks. An MAOI is a medicine sometimes used for depression and other mental problems. Examples of MAOI medicines are Nardil® (phenylzine sulfate) and Parnate® (tranylcypromine sulfate). Taking SYMBYAX with a MAOI may cause serious side effects that can be life threatening. Do not take a MAOI for at least 5 weeks after you stop taking SYMBYAX.
- Taking Mellaril® (thioridazine) for mental problems or stopped taking it within the last 5 weeks. Mellaril® (thioridazine) can cause a heart problem (prolongation of the QTc interval) that can cause death. SYMBYAX with Mellaril® (thioridazine) can increase your chances of having this serious and life-threatening heart problem.
- Allergic to SYMBYAX or any of its ingredients. The active ingredients are olanzapine and fluoxetine hydrochloride. See the end of this leaflet for a complete list of ingredients in SYMBYAX.
What should I tell my doctor before taking SYMBYAX?
- Tell your doctor if you are taking fluoxetine, Prozac, Prozac Weekly, Sarafem, olanzapine, Zyprexa, or Zyprexa Zydis. These medicines each contain an active ingredient that is also found in SYMBYAX.
- Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. SYMBYAX can interact with many other medicines, causing serious or life-threatening side effects. Your doctor will decide if you can take SYMBYAX with your other medicines, or if your dose should be adjusted. Keep a list of your medicines with you and show it to your doctor and pharmacist every time you are prescribed a new medicine or start a new non-prescription medicine, vitamin, or herbal supplement.
- Tell your doctor if you are taking SYMBYAX and are taking or plan to take nonsteroidal anti-inflammatory drugs or aspirin since combined use of these drug products has been associated with an increased risk of bleeding.
Before taking SYMBYAX, tell your doctor if you have or had the following medical conditions:
- Are pregnant or plan to become pregnant. It is not known if SYMBYAX can harm your unborn baby. You and your doctor should decide if SYMBYAX is right for you during pregnancy.
- Are breast-feeding or plan to breast-feed. SYMBYAX may pass into your milk and may harm your baby. You should choose either to breast-feed or take SYMBYAX, but not both.
- Are older than age 65 and have a mental problem called dementia (slow loss of mental function)
- High blood sugar, diabetes or family history of diabetes
- Liver problems. You may need a lower dose of SYMBYAX.
- Seizures (convulsions or fits)
- Low blood pressure. SYMBYAX may cause dizziness or fainting in people with low blood pressure.
- Heart problems including heart attacks
- Strokes, or mini-strokes called transient ischemic attacks (TIA)
- High blood pressure
- An enlarged prostate (men)
- An eye problem called narrow angle glaucoma
- A stomach problem called a paralytic ileus
Also, tell your doctor if you
- Currently smoke
- Drink alcohol, especially if you drink a lot
- Exercise a lot or are often in hot places
How should I take SYMBYAX?
- Take SYMBYAX exactly as instructed by your doctor. Your doctor will usually start youon a low dose of SYMBYAX. Your dose may be adjusted depending on your body s response to SYMBYAX. Your dose will also depend on certain medical problems you have. Do not stop taking SYMBYAX or change your dose even if you feel better, without talking with your doctor.
- SYMBYAX is usually taken once a day in the evening. Take SYMBYAX at the sametime each day. SYMBYAX may be taken with or without food.
- If you miss a dose, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and take only your regularly scheduled dose. Do not take more than your doctor has prescribed for you.
- Tell your doctor if your depression does not get better while taking SYMBYAX. Your doctor may adjust your dose or give you a different medicine.
- If you take too much SYMBYAX or overdose, call your doctor or poison control center right away, or go to the nearest emergency room.
What should I avoid while taking SYMBYAX?
- Do not drive or operate other dangerous machinery until you know how SYMBYAX affects you. SYMBYAX can impair your judgment, thinking, and motor skills.
- Do not take medicines, including prescription and non-prescription medicines, vitaminsand herbal supplements unless you have talked to your doctor about them.
- Do not get pregnant.
- Do not breast-feed.
- Do not drink alcohol.
- Do not get over-heated or dehydrated (loss of body fluids) during hot weather or exercise,or when using a hot tub.
- Do not take a MAOI medicine for at least 5 weeks after you stop taking SYMBYAX.
What are the possible side effects of SYMBYAX?
All medicines may cause side effects in some patients. Serious side effects reported by patients treated with SYMBYAX follow below:
- Severe allergic reactions that cause hives, swelling of your face, eyes, mouth, or tongue, trouble breathing or a rash with fever and joint pain. Tell your doctor right away if you get these symptoms. Your doctor may stop SYMBYAX and prescribe medicines to treat your allergic reaction.
- Strokes and "mini-strokes" called transient ischemic attacks (TIAs). These are more common in elderly patients with dementia. As with other mental health drugs, SYMBYAX should be used with caution in elderly patients with dementia. SYMBYAX is not approved for the treatment of elderly patients with dementia.
- High blood sugar or diabetes. Patients who already have diabetes should have their blood sugar checked regularly during treatment with SYMBYAX. Patients at risk for diabetes (for example, those who are overweight or have a family history of diabetes) who are starting treatment with SYMBYAX should undergo blood sugar testing on an empty stomach at the beginning of treatment and regularly during treatment. Any patient treated with SYMBYAX should be monitored for signs of high blood sugar including being thirsty, going to the bathroom a lot, eating a lot, and feeling weak. Patients who develop signs of high blood sugar during treatment with SYMBYAX should undergo blood sugar testing on an empty stomach. In some cases, high blood sugar has gone away when SYMBYAX was stopped; however, some patients had to keep taking medicine for diabetes even though they stopped taking SYMBYAX.
- Neuroleptic malignant syndrome (NMS). NMS is a rare, but life-threatening reaction to certain medicines for mental problems, including SYMBYAX. Stop taking SYMBYAX and call your doctor right away if you get any of the following symptoms of NMS, such as a high fever, sweating, muscle stiffness, trouble thinking clearly, a change in mental functioning, sleepiness, or changes in your breathing, heartbeat, and blood pressure. NMS can cause death and must be treated in a hospital.
- Tardive dyskinesia. This is a condition caused by certain medicines for mental problems, including SYMBYAX. It causes body movements, mostly in your face or tongue, that keep happening and that you cannot control. It may start after you stop taking SYMBYAX. Tardive dyskinesia may not go away, even if you stop taking SYMBYAX. Tell your doctor if you get body movements that you can t control.
- Low blood pressure. SYMBYAX may cause low blood pressure in some patients. Low blood pressure is more likely in patients who have heart problems, who have brain problems such as strokes, who take certain medicines, or who drink alcohol. Signs of low blood pressure include dizziness, fast heartbeat, and fainting. To lower your chances of fainting while taking SYMBYAX, stand up slowly if you have been sitting or lying down.
- Seizures. SYMBYAX should be used cautiously in people who have had seizures in the past or who have conditions that increase their risk for seizures.
- Impaired judgment, thinking, and motor skills
- Trouble swallowing
- Abnormal bleeding. When SYMBYAX is used alone, and especially with certain other medicines that can increase bleeding risk (for example; ibuprofen or aspirin), your risk of bleeding can increase. If you notice increased or unusual bruising or other bleeding, contact your doctor.
- Low salt levels in the blood. SYMBYAX can cause a low salt level in the blood. Weakness, confusion, or trouble thinking can be caused by low salt levels in the blood. If you develop any of these symptoms, contact your doctor.
- Body temperature problems. SYMBYAX can cause problems in keeping your body temperature regular. Do not become overheated or dehydrated during hot weather or exercise, or when using a hot tub.
Common side effects of SYMBYAX are:
- Weight gain
- Sleepiness
- Diarrhea
- Dry mouth
- Increased appetite
- Feeling weak
- Swelling of your hands and feet
- Tremors (shakes)
- Sore throat
- Trouble concentrating
- SYMBYAX can cause problems in keeping your body temperature regulated. Tell your doctor about any side effect that bothers you or won t go away. Your doctor may be able to help you manage the side effect. These are not all the side effects of SYMBYAX. For more information ask your doctor or pharmacist.
Other important safety information about SYMBYAX
- The symptoms of bipolar disorder may include thoughts of harming yourself or others orcommitting suicide. Tell your doctor immediately or go to an emergency center if you have any of these thoughts. Symptoms of bipolar disorder may include mania. If you experience manic symptoms (forexample; racing thoughts, poor sleep, irritability, mood swings, extra energy), contact your doctor.
- If your depression becomes worse, contact your doctor.
- Rarely, people taking medicines of this type have started to leak milk from their breasts, and women have missed periods or had irregular periods. If these symptoms occur, contact your doctor.
- If you gain weight while taking SYMBYAX, contact your doctor to discuss changes youcan make in your activities or eating habits to help manage your weight.
- Problems with sexual functioning have commonly occurred in patients taking SYMBYAX. If these symptoms occur, contact your doctor.
How do I store SYMBYAX?
- Store SYMBYAX at room temperature, 59° to 86°F (15° to 30°C).
- Keep the container tightly closed and protect from moisture.
- Keep SYMBYAX and all medicines away from children.
General information about SYMBYAX
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not take SYMBYAX for a condition for which it was not prescribed. Do not give SYMBYAX to other people, even if they have the same symptoms that you have. It may harm them.
This leaflet summarizes important information about SYMBYAX. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information that is written for health professionals. You can also call 1-800-Lilly-Rx (1-800-545-5979) or visit our website at www.SYMBYAX.com.
What are the ingredients in SYMBYAX?
Active ingredients: olanzapine and fluoxetine hydrochloride
Inactive ingredients: pregelatinized starch, gelatin, dimethicone, titanium dioxide, sodium lauryl sulfate, edible black ink, red iron oxide, yellow iron oxide, and/or black iron oxide.
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with SYMBYAX and should counsel them in its appropriate use. A patient Medication Guide About Using Antidepressants in Children and Teenagers is available for SYMBYAX. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking SYMBYAX.
Clinical Worsening and Suicide Risk - Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to observe for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
Abnormal Bleeding - Patients should be cautioned about the concomitant use of SYMBYAX and NSAIDs, aspirin, or other drugs that affect coagulation since the combined use of psychotropic drugs that interfere with serotonin reuptake and these agents has been associated with an increased risk of bleeding (see PRECAUTIONS, Abnormal Bleeding).
Alcohol - Patients should be advised to avoid alcohol while taking SYMBYAX.
Cognitive and Motor Impairment - As with any CNS-active drug, SYMBYAX has the potential to impair judgment, thinking, or motor skills. Patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that SYMBYAX therapy does not affect them adversely.
Concomitant Medication - Patients should be advised to inform their physician if they are taking Prozac®, Prozac Weekly™,, Sarafem®, fluoxetine, Zyprexa®, or Zyprexa Zydis®. Patients should also be advised to inform their physicians if they are taking or plan to take any prescription or over-the-counter drugs, including herbal supplements, since there is a potential for interactions.
Heat Exposure and Dehydration - Patients should be advised regarding appropriate care in avoiding overheating and dehydration.
Nursing - Patients, if taking SYMBYAX, should be advised not to breast-feed.
Orthostatic Hypotension - Patients should be advised of the risk of orthostatic hypotension, especially during the period of initial dose titration and in association with the use of concomitant drugs that may potentiate the orthostatic effect of olanzapine, e.g., diazepam or alcohol (see WARNINGS and Drug Interactions).
Pregnancy - Patients should be advised to notify their physician if they become pregnant or intend to become pregnant during SYMBYAX therapy.
Rash - Patients should be advised to notify their physician if they develop a rash or hives while taking SYMBYAX.
Treatment Adherence - Patients should be advised to take SYMBYAX exactly as prescribed, and to continue taking SYMBYAX as prescribed even after their mood symptoms improve. Patients should be advised that they should not alter their dosing regimen, or stop taking SYMBYAX, without consulting their physician.
Patient information is printed at the end of this insert. Physicians should discuss this information with their patients and instruct them to read the Medication Guide before starting therapy with SYMBYAX and each time their prescription is refilled.
Laboratory Tests
Periodic assessment of transaminases is recommended in patients with significant hepatic disease (see Transaminase Elevations).
DRUG INTERACTIONS
The risks of using SYMBYAX in combination with other drugs have not been extensively evaluated in systematic studies. The drug-drug interactions of the individual components are applicable to SYMBYAX. As with all drugs, the potential for interaction by a variety of mechanisms (e.g., pharmacodynamic, pharmacokinetic drug inhibition or enhancement, etc.) is a possibility. Caution is advised if the concomitant administration of SYMBYAX and other CNS-active drugs is required. In evaluating individual cases, consideration should be given to using lower initial doses of the concomitantly administered drugs, using conservative titration schedules, and monitoring of clinical status (see CLINICAL PHARMACOLOGY, Accumulation and slow elimination).
Antihypertensive agents - Because of the potential for olanzapine to induce hypotension, SYMBYAX may enhance the effects of certain antihypertensive agents (see WARNINGS, Orthostatic Hypotension).
Anti-Parkinsonian - The olanzapine component of SYMBYAX may antagonize the effects of levodopa and dopamine agonists.
Benzodiazepines - Multiple doses of olanzapine did not influence the pharmacokinetics of diazepam and its active metabolite N-desmethyldiazepam. However, the coadministration of diazepam with olanzapine potentiated the orthostatic hypotension observed with olanzapine.
When concurrently administered with fluoxetine, the half-life of diazepam may be prolonged in some patients (see CLINICAL PHARMACOLOGY, Accumulation and slow elimination). Coadministration of alprazolam and fluoxetine has resulted in increased alprazolam plasma concentrations and in further psychomotor performance decrement due to increased alprazolam levels.
Biperiden - Multiple doses of olanzapine did not influence the pharmacokinetics of biperiden.
Carbamazepine - Carbamazepine therapy (200 mg BID) causes an approximate 50% increase in the clearance of olanzapine. This increase is likely due to the fact that carbamazepine is a potent inducer of CYP1A2 activity. Higher daily doses of carbamazepine may cause an even greater increase in olanzapine clearance.
Patients on stable doses of carbamazepine have developed elevated plasma anticonvulsant concentrations and clinical anticonvulsant toxicity following initiation of concomitant fluoxetine treatment.
Clozapine - Elevation of blood levels of clozapine has been observed in patients receiving concomitant fluoxetine.
Electroconvulsive therapy (ECT) - There are no clinical studies establishing the benefit of the combined use of ECT and fluoxetine. There have been rare reports of prolonged seizures in patients on fluoxetine receiving ECT treatment (see Seizures).
Ethanol - Ethanol (45 mg/70 kg single dose) did not have an effect on olanzapine pharmacokinetics. The coadministration of ethanol with SYMBYAX may potentiate sedation and orthostatic hypotension.
Fluvoxamine - Fluvoxamine, a CYP1A2 inhibitor, decreases the clearance of olanzapine. This results in a mean increase in olanzapine Cmax following fluvoxamine administration of 54% in female nonsmokers and 77% in male smokers. The mean increase in olanzapine AUC is 52% and 108%, respectively. Lower doses of the olanzapine component of SYMBYAX should be considered in patients receiving concomitant treatment with fluvoxamine.
Haloperidol - Elevation of blood levels of haloperidol has been observed in patients receiving concomitant fluoxetine.
Lithium - Multiple doses of olanzapine did not influence the pharmacokinetics of lithium.
There have been reports of both increased and decreased lithium levels when lithium was used concomitantly with fluoxetine. Cases of lithium toxicity and increased serotonergic effects have been reported. Lithium levels should be monitored in patients taking SYMBYAX concomitantly with lithium.
Monoamine oxidase inhibitors - See CONTRAINDICATIONS.
Phenytoin - Patients on stable doses of phenytoin have developed elevated plasma levels of phenytoin with clinical phenytoin toxicity following initiation of concomitant fluoxetine.
Pimozide - A single case report has suggested possible additive effects of pimozide and fluoxetine leading to bradycardia.
Sumatriptan - There have been rare postmarketing reports describing patients with weakness, hyperreflexia, and incoordination following the use of an SSRI and sumatriptan. If concomitant treatment with sumatriptan and an SSRI (e.g., fluoxetine, fluvoxamine, paroxetine, sertraline, or citalopram) is clinically warranted, appropriate observation of the patient is advised.
Theophylline - Multiple doses of olanzapine did not affect the pharmacokinetics of theophylline or its metabolites.
Thioridazine - See CONTRAINDICATIONS and WARNINGS, Thioridazine.
Tricyclic antidepressants (TCAs) - Single doses of olanzapine did not affect the pharmacokinetics of imipramine or its active metabolite desipramine.
In two fluoxetine studies, previously stable plasma levels of imipramine and desipramine have increased >2- to 10-fold when fluoxetine has been administered in combination. This influence may persist for three weeks or longer after fluoxetine is discontinued. Thus, the dose of TCA may need to be reduced and plasma TCA concentrations may need to be monitored temporarily when SYMBYAX is coadministered or has been recently discontinued (see Drugs metabolized by CYP2D6 and CLINICAL PHARMACOLOGY, Accumulation and slow elimination).
Tryptophan - Five patients receiving fluoxetine in combination with tryptophan experienced adverse reactions, including agitation, restlessness, and gastrointestinal distress.
Valproate - In vitro studies using human liver microsomes determined that olanzapine has little potential to inhibit the major metabolic pathway, glucuronidation, of valproate. Further, valproate has little effect on the metabolism of olanzapine in vitro. Thus, a clinically significant pharmacokinetic interaction between olanzapine and valproate is unlikely.
Warfarin - Warfarin (20-mg single dose) did not affect olanzapine pharmacokinetics. Single doses of olanzapine did not affect the pharmacokinetics of warfarin.
Altered anticoagulant effects, including increased bleeding, have been reported when fluoxetine is coadministered with warfarin (see PRECAUTIONS, Abnormal Bleeding). Patients receiving warfarin therapy should receive careful coagulation monitoring when SYMBYAX is initiated or stopped.
Drugs that interfere with hemostasis (NSAIDs, aspirin, warfarin, etc.) - Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies of the case-control and cohort design that have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding have also shown that concurrent use of an NSAID or aspirin potentiated the risk of bleeding (see PRECAUTIONS, Abnormal Bleeding). Thus, patients should be cautioned about the use of such drugs concurrently with SYMBYAX.
Drugs metabolized by CYP2D6 - In vitro studies utilizing human liver microsomes suggest that olanzapine has little potential to inhibit CYP2D6. Thus, olanzapine is unlikely to cause clinically important drug interactions mediated by this enzyme.
Approximately 7% of the normal population has a genetic variation that leads to reduced levels of activity of CYP2D6. Such individuals have been referred to as poor metabolizers of drugs such as debrisoquin, dextromethorphan, and TCAs. Many drugs, such as most antidepressants, including fluoxetine and other selective uptake inhibitors of serotonin, are metabolized by this isoenzyme; thus, both the pharmacokinetic properties and relative proportion of metabolites are altered in poor metabolizers. However, for fluoxetine and its metabolite, the sum of the plasma concentrations of the 4 enantiomers is comparable between poor and extensive metabolizers (see CLINICAL PHARMACOLOGY, Variability in metabolism).
Fluoxetine, like other agents that are metabolized by CYP2D6, inhibits the activity of this isoenzyme, and thus may make normal metabolizers resemble poor metabolizers. Therapy with medications that are predominantly metabolized by the CYP2D6 system and that have a relatively narrow therapeutic index should be initiated at the low end of the dose range if a patient is receiving fluoxetine concurrently or has taken it in the previous five weeks. If fluoxetine is added to the treatment regimen of a patient already receiving a drug metabolized by CYP2D6, the need for a decreased dose of the original medication should be considered. Drugs with a narrow therapeutic index represent the greatest concern (including but not limited to, flecainide, vinblastine, and TCAs). Due to the risk of serious ventricular arrhythmias and sudden death potentially associated with elevated thioridazine plasma levels, thioridazine should not be administered with fluoxetine or within a minimum of five weeks after fluoxetine has been discontinued (see CONTRAINDICATIONS, Monoamine Oxidase Inhibitors (MAOI) and WARNINGS, Thioridazine).
Drugs metabolized by CYP3A - In vitro studies utilizing human liver microsomes suggest that olanzapine has little potential to inhibit CYP3A. Thus, olanzapine is unlikely to cause clinically important drug interactions mediated by these enzymes.
In an in vivo interaction study involving the coadministration of fluoxetine with single doses of terfenadine (a CYP3A substrate), no increase in plasma terfenadine concentrations occurred with concomitant fluoxetine. In addition, in vitro studies have shown ketoconazole, a potent inhibitor of CYP3A activity, to be at least 100 times more potent than fluoxetine or norfluoxetine as an inhibitor of the metabolism of several substrates for this enzyme, including astemizole, cisapride, and midazolam. These data indicate that fluoxetine's extent of inhibition of CYP3A activity is not likely to be of clinical significance.
Effect of olanzapine on drugs metabolized by other CYP enzymes - In vitro studies utilizing human liver microsomes suggest that olanzapine has little potential to inhibit CYP1A2, CYP2C9, and CYP2C19. Thus, olanzapine is unlikely to cause clinically important drug interactions mediated by these enzymes.
The effect of other drugs on olanzapine - Fluoxetine, an inhibitor of CYP2D6, decreases olanzapine clearance a small amount (see CLINICAL PHARMACOLOGY, Pharmacokinetics). Agents that induce CYP1A2 or glucuronyl transferase enzymes, such as omeprazole and rifampin, may cause an increase in olanzapine clearance. Fluvoxamine, an inhibitor of CYP1A2, decreases olanzapine clearance (see Drug Interactions, Fluvoxamine). The effect of CYP1A2 inhibitors, such as fluvoxamine and some fluoroquinolone antibiotics, on SYMBYAX has not been evaluated. Although olanzapine is metabolized by multiple enzyme systems, induction or inhibition of a single enzyme may appreciably alter olanzapine clearance. Therefore, a dosage increase (for induction) or a dosage decrease (for inhibition) may need to be considered with specific drugs.
Drugs tightly bound to plasma proteins - The in vitro binding of SYMBYAX to human plasma proteins is similar to the individual components. The interaction between SYMBYAX and other highly protein-bound drugs has not been fully evaluated. Because fluoxetine is tightly bound to plasma protein, the administration of fluoxetine to a patient taking another drug that is tightly bound to protein (e.g., Coumadin, digitoxin) may cause a shift in plasma concentrations potentially resulting in an adverse effect. Conversely, adverse effects may result from displacement of protein-bound fluoxetine by other tightly bound drugs (see CLINICAL PHARMACOLOGY, Distribution and PRECAUTIONS, Drug Interactions).
Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity, mutagenicity, or fertility studies were conducted with SYMBYAX. The following data are based on findings in studies performed with the individual components.
Carcinogenesis
Olanzapine - Oral carcinogenicity studies were conducted in mice and rats. Olanzapine was administered to mice in two 78-week studies at doses of 3, 10, and 30/20 mg/kg/day [equivalent to 0.8 to 5 times the maximum recommended human daily dose (MRHD) on a mg/m2 basis] and 0.25, 2, and 8 mg/kg/day (equivalent to 0.06 to 2 times the MRHD on a mg/m2 basis). Rats were dosed for 2 years at doses of 0.25, 1, 2.5, and 4 mg/kg/day (males) and 0.25, 1, 4, and 8 mg/kg/day (females) (equivalent to 0.1 to 2 and 0.1 to 4 times the MRHD on a mg/m2 basis, respectively). The incidence of liver hemangiomas and hemangiosarcomas was significantly increased in one mouse study in females dosed at 8 mg/kg/day (2 times the MRHD on a mg/m2 basis). These tumors were not increased in another mouse study in females dosed at 10 or 30/20 mg/kg/day (2 to 5 times the MRHD on a mg/m2 basis); in this study, there was a high incidence of early mortalities in males of the 30/20 mg/kg/day group. The incidence of mammary gland adenomas and adenocarcinomas was significantly increased in female mice dosed at =2 mg/kg/day and in female rats dosed at =4 mg/kg/day (0.5 and 2 times the MRHD on a mg/m2 basis, respectively). Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the olanzapine carcinogenicity studies; however, measurements during subchronic toxicity studies showed that olanzapine elevated serum prolactin levels up to 4-fold in rats at the same doses used in the carcinogenicity study. An increase in mammary gland neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin-mediated. The relevance for human risk of the finding of prolactin-mediated endocrine tumors in rodents is unknown (see PRECAUTIONS, Hyperprolactinemia).
Fluoxetine - The dietary administration of fluoxetine to rats and mice for two years at doses of up to 10 and 12 mg/kg/day, respectively (approximately 1.2 and 0.7 times, respectively, the MRHD on a mg/m2 basis), produced no evidence of carcinogenicity.
Mutagenesis
Olanzapine - No evidence of mutagenic potential for olanzapine was found in the Ames reverse mutation test, in vivo micronucleus test in mice, the chromosomal aberration test in Chinese hamster ovary cells, unscheduled DNA synthesis test in rat hepatocytes, induction of forward mutation test in mouse lymphoma cells, or in vivo sister chromatid exchange test in bone marrow of Chinese hamsters.
Fluoxetine - Fluoxetine and norfluoxetine have been shown to have no genotoxic effects based on the following assays: bacterial mutation assay, DNA repair assay in cultured rat hepatocytes, mouse lymphoma assay, and in vivo sister chromatid exchange assay in Chinese hamster bone marrow cells.
Impairment of Fertility
SYMBYAX - Fertility studies were not conducted with SYMBYAX. However, in a repeat-dose rat toxicology study of three months duration, ovary weight was decreased in females treated with the low-dose [2 and 4 mg/kg/day (1 and 0.5 times the MRHD on a mg/m2 basis), respectively] and high-dose [4 and 8 mg/kg/day (2 and 1 times the MRHD on a mg/m2 basis), respectively] combinations of olanzapine and fluoxetine. Decreased ovary weight, and corpora luteal depletion and uterine atrophy were observed to a greater extent in the females receiving the high-dose combination than in females receiving either olanzapine or fluoxetine alone. In a 3-month repeat-dose dog toxicology study, reduced epididymal sperm and reduced testicular and prostate weights were observed with the high-dose combination of olanzapine and fluoxetine [5 and 5 mg/kg/day (9 and 2 times the MRHD on a mg/m2 basis), respectively] and with olanzapine alone (5 mg/kg/day or 9 times the MRHD on a mg/m2 basis).
Olanzapine - In a fertility and reproductive performance study in rats, male mating performance, but not fertility, was impaired at a dose of 22.4 mg/kg/day and female fertility was decreased at a dose of 3 mg/kg/day (11 and 1.5 times the MRHD on a mg/m2 basis, respectively). Discontinuance of olanzapine treatment reversed the effects on male-mating performance. In female rats, the precoital period was increased and the mating index reduced at 5 mg/kg/day (2.5 times the MRHD on a mg/m2 basis). Diestrous was prolonged and estrous was delayed at 1.1 mg/kg/day (0.6 times the MRHD on a mg/m2 basis); therefore, olanzapine may produce a delay in ovulation.
Fluoxetine - Two fertility studies conducted in adult rats at doses of up to 7.5 and 12.5 mg/kg/day (approximately 0.9 and 1.5 times the MRHD on a mg/m2 basis) indicated that fluoxetine had no adverse effects on fertility (see ANIMAL TOXICOLOGY).
Pregnancy - Pregnancy Category C
SYMBYAX
Embryo fetal development studies were conducted in rats and rabbits with olanzapine and fluoxetine in low-dose and high-dose combinations. In rats, the doses were: 2 and 4 mg/kg/day (low-dose) [1 and 0.5 times the MRHD on a mg/m2 basis, respectively], and 4 and 8 mg/kg/day (high-dose) [2 and 1 times the MRHD on a mg/m2 basis, respectively]. In rabbits, the doses were 4 and 4 mg/kg/day (low-dose) [4 and 1 times the MRHD on a mg/m2 basis, respectively], and 8 and 8 mg/kg/day (high-dose) [9 and 2 times the MRHD on a mg/m2 basis, respectively]. In these studies, olanzapine and fluoxetine were also administered alone at the high-doses (4 and 8 mg/kg/day, respectively, in the rat; 8 and 8 mg/kg/day, respectively, in the rabbit). In the rabbit, there was no evidence of teratogenicity; however, the high-dose combination produced decreases in fetal weight and retarded skeletal ossification in conjunction with maternal toxicity. Similarly, in the rat there was no evidence of teratogenicity; however, a decrease in fetal weight was observed with the high-dose combination.
In a pre- and postnatal study conducted in rats, olanzapine and fluoxetine were administered during pregnancy and throughout lactation in combination (low-dose: 2 and 4 mg/kg/day [1 and 0.5 times the MRHD on a mg/m2 basis], respectively, high-dose: 4 and 8 mg/kg/day [2 and 1 times the MRHD on a mg/m2 basis], respectively, and alone: 4 and 8 mg/kg/day [2 and 1 times the MRHD on a mg/m2 basis], respectively). Administration of the high-dose combination resulted in a marked elevation in offspring mortality and growth retardation in comparison to the same doses of olanzapine and fluoxetine administered alone. These effects were not observed with the low-dose combination; however, there were a few cases of testicular degeneration and atrophy, depletion of epididymal sperm and infertility in the male progeny. The effects of the high-dose combination on postnatal endpoints could not be assessed due to high progeny mortality.
There are no adequate and well-controlled studies with SYMBYAX in pregnant women.
SYMBYAX should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Olanzapine
In reproduction studies in rats at doses up to 18 mg/kg/day and in rabbits at doses up to 30 mg/kg/day (9 and 30 times the MRHD on a mg/m2 basis, respectively), no evidence of teratogenicity was observed. In a rat teratology study, early resorptions and increased numbers of nonviable fetuses were observed at a dose of 18 mg/kg/day (9 times the MRHD on a mg/m2 basis). Gestation was prolonged at 10 mg/kg/day (5 times the MRHD on a mg/m2 basis). In a rabbit teratology study, fetal toxicity (manifested as increased resorptions and decreased fetal weight) occurred at a maternally toxic dose of 30 mg/kg/day (30 times the MRHD on a mg/m2 basis).
Placental transfer of olanzapine occurs in rat pups.
There are no adequate and well-controlled clinical studies with olanzapine in pregnant women. Seven pregnancies were observed during premarketing clinical studies with olanzapine, including two resulting in normal births, one resulting in neonatal death due to a cardiovascular defect, three therapeutic abortions, and one spontaneous abortion.
Fluoxetine
In embryo fetal development studies in rats and rabbits, there was no evidence of teratogenicity following administration of up to 12.5 and 15 mg/kg/day, respectively (1.5 and 3.6 times the MRHD on a mg/m2 basis, respectively) throughout organogenesis. However, in rat reproduction studies, an increase in stillborn pups, a decrease in pup weight, and an increase in pup deaths during the first 7 days postpartum occurred following maternal exposure to 12 mg/kg/day (1.5 times the MRHD on a mg/m2 basis) during gestation or 7.5 mg/kg/day (0.9 times the MRHD on a mg/m2 basis) during gestation and lactation. There was no evidence of developmental neurotoxicity in the surviving offspring of rats treated with 12 mg/kg/day during gestation. The no-effect dose for rat pup mortality was 5 mg/kg/day (0.6 times the MRHD on a mg/m2 basis).
Nonteratogenic Effects - Neonates exposed to fluoxetine and other SSRIs or serotonin and norepinephrine reuptake inhibitors (SNRIs), late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These features are consistent with either a direct toxic effect of SSRIs and SNRIs or, possibly, a drug discontinuation syndrome. It should be noted that, in some cases, the clinical picture is consistent with serotonin syndrome (see CONTRAINDICATIONS, Monoamine Oxidase Inhibitors). When treating a pregnant woman with fluoxetine during the third trimester, the physician should carefully consider the potential risks and benefits of treatment (see DOSAGE AND ADMINISTRATION).
Labor and Delivery
SYMBYAX
The effect of SYMBYAX on labor and delivery in humans is unknown. Parturition in rats was not affected by SYMBYAX. SYMBYAX should be used during labor and delivery only if the potential benefit justifies the potential risk.
Olanzapine
Parturition in rats was not affected by olanzapine. The effect of olanzapine on labor and delivery in humans is unknown.
Fluoxetine
The effect of fluoxetine on labor and delivery in humans is unknown. Fluoxetine crosses the placenta; therefore, there is a possibility that fluoxetine may have adverse effects on the newborn.
Nursing Mothers
SYMBYAX
There are no adequate and well-controlled studies with SYMBYAX in nursing mothers or infants. No studies have been conducted to examine the excretion of olanzapine or fluoxetine in breast milk following SYMBYAX treatment. It is recommended that women not breast-feed when receiving SYMBYAX.
Olanzapine
Olanzapine was excreted in milk of treated rats during lactation.
Fluoxetine
Fluoxetine is excreted in human breast milk. In one breast milk sample, the concentration of fluoxetine plus norfluoxetine was 70.4 ng/mL. The concentration in the mother's plasma was 295.0 ng/mL. No adverse effects on the infant were reported. In another case, an infant nursed by a mother on fluoxetine developed crying, sleep disturbance, vomiting, and watery stools. The infant's plasma drug levels were 340 ng/mL of fluoxetine and 208 ng/mL of norfluoxetine on the 2nd day of feeding.
Pediatric Use
Safety and effectiveness in the pediatric population have not been established (see BOX WARNING, WARNINGS, Clinical Worsening and Suicide Risk and ANIMAL TOXICOLOGY). Anyone considering the use of SYMBYAX in a child or adolescent must balance the potential risks with the clinical need. and
Geriatric Use
SYMBYAX
Clinical studies of SYMBYAX did not include sufficient numbers of patients à ¢Ã¢â‚¬°Ã‚ ¥65 years of age to determine whether they respond differently from younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy (see DOSAGE AND ADMINISTRATION).
Olanzapine
Of the 2500 patients in premarketing clinical studies with olanzapine, 11% (263 patients) were ≥65 years of age. In patients with schizophrenia, there was no indication of any different tolerability of olanzapine in the elderly compared with younger patients. Studies in patients with dementia-related psychosis have suggested that there may be a different tolerability profile in this population compared with younger patients with schizophrenia. In placebo-controlled studies of olanzapine in elderly patients with dementia-related psychosis, there was a significantly higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack) in patients treated with olanzapine compared to patients treated with placebo. Olanzapine is not approved for the treatment of patients with dementia-related psychosis. If the prescriber elects to treat elderly patients with dementia-related psychosis, vigilance should be exercised (see WARNINGS, Safety Experience in Elderly Patients with Dementia-Related Psychosis, PRECAUTIONS, Use in Patients with Concomitant Illness and DOSAGE AND ADMINISTRATION, Special Populations).
As with other CNS-active drugs, olanzapine should be used with caution in elderly patients with dementia. Also, the presence of factors that might decrease pharmacokinetic clearance or increase the pharmacodynamic response to olanzapine should lead to consideration of a lower starting dose for any geriatric patient.
Fluoxetine
US fluoxetine clinical studies (10,782 patients) included 687 patients ≥65 years of age and 93 patients ≥75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. As with other SSRIs, fluoxetine has been associated with cases of clinically significant hyponatremia in elderly patients.
Eli Lilly and Company
Indianapolis, IN 46285
www.SYMBYAX.com
Full Symbyax Prescribing Information
Symbyax Medication Guide
The information in this monograph is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects. This information is generalized and is not intended as specific medical advice. If you have questions about the medicines you are taking or would like more information, check with your doctor, pharmacist, or nurse.
APA Reference
Staff, H.
(2009, January 4). Symbyax Patient Information, HealthyPlace. Retrieved
on 2026, January 14 from https://www.healthyplace.com/other-info/psychiatric-medications/symbyax-patient-information