The Psychopathic Brain: Is It Different from a Normal Brain?

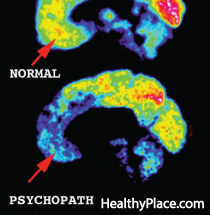
The psychopathic brain has been an interest of study for decades due to the fact that psychopaths represent such a small segment of society and yet commit a highly disproportionate amount of criminal acts (like these famous psychopaths and psychopath killers). And with more-and-more psychopaths having magnetic resonance imaging (MRI) scans or functional MRI (fMRI) scans, some correlates have been found. In short, the brain of a psychopath is different than a normal brain.
There are three main parts of the brain which psychopath brain scans show significant differences in. They are in the regions of the amygdala, the prefrontal cortex, and the extended paralimbic structures. Light is shed on these regions in the paper, The Psychopath Magnetized: Insights from Brain Imaging, by Anderson and Kiehl. The effects on these regions of the brain may be what produces psychopathic symptoms and what is termed the psychopathic personality.
The Brain of a Psychopath: The Amygdala
The amygdala in critical in the acquisition of information around us that reinforces learning. Learning, for example, is what teaches us what societal norms are and without that, we may be more prone to antisocial behavior like a psychopath. The amygdala also allows for the recognition of emotionally important information, such as the presence of threats.
In recent studies, psychopathic brains showed less activation in the amygdala when viewing pictures depicting moral violations and fearful faces; suggesting these things simply affect a psychopathic brain less. The greater the level of psychopathy, as measured on the Hare Psychopathic Checklist (psychopath test), the less the activation seen in the amygdala.
The Brain of a Psychopath: The Prefrontal Cortex
Areas of the prefrontal cortex are important in monitoring our behavior, estimating consequences and incorporating emotional learning into our future decision-making process. If this area is deficient, this could mean that, for psychopaths, whatever they would learn through emotions would not affect future decisions and they may underestimate the consequences of their actions.
A section of the prefrontal cortex – the orbitofrontal cortex – shows reduced grey matter in volume and thickness. Again, the more severe the psychopathy, the greater this deficiency seems to be. The activation in this region during specific tasks mirrors this finding as when psychopaths decide to cooperate, they show less activation here and when they observe an opponent being punished, this area activates more than in the normal brain (which correlates with antisocial behavior and impulsivity traits).
The Brain of a Psychopath: Extended Paralimbic Structures
Recent research has shown that the dysfunction in a psychopathic brain goes beyond the mere limbic system as above and into the areas around the limbic system as well. This may indicate broader cognitive impairments in general.
In these other regions of the brain, volume reduction has also be found and these reductions have been linked to impairments in episodic memory and in self-referential experiences perhaps meaning that psychopaths view their own memories differently than do others and perhaps see their roles in those memories differently (perhaps as more grandiose). The deficits in emotions seen in psychopaths have also been linked to decreased grey matter volume in parts of the brain.
APA Reference
Tracy, N.
(2021, December 17). The Psychopathic Brain: Is It Different from a Normal Brain?, HealthyPlace. Retrieved
on 2026, March 9 from https://www.healthyplace.com/personality-disorders/psychopath/the-psychopathic-brain-is-it-different-from-a-normal-brain



