Decoding Schizophrenia
A fuller understanding of signaling in the brain of people with schizophrenia offers new hope for improved therapy
Today the word "schizophrenia" brings to mind such names as John Nash and Andrea Yates. Nash, the subject of the Oscar-winning film A Beautiful Mind, emerged as a mathematical prodigy and eventually won a Nobel Prize for his early work, but he became so profoundly disturbed by the brain disorder in young adulthood that he lost his academic career and floundered for years before recovering. Yates, a mother of five who suffers from both depression and schizophrenia, infamously drowned her young children in a bathtub to "save them from the devil" and is now in prison.
The experiences of Nash and Yates are typical in some ways but atypical in others. Of the roughly 1 percent of the world's population stricken with schizophrenia, most remain largely disabled throughout adulthood. Rather than being geniuses like Nash, many show below- average intelligence even before they become symptomatic and then undergo a further decline in IQ when the illness sets in, typically during young adulthood. Unfortunately, only a minority ever achieve gainful employment. In contrast to Yates, fewer than half marry or raise families. Some 15 percent reside for long periods in state or county mental health facilities, and another 15 percent end up incarcerated for petty crimes and vagrancy. Roughly 60 percent live in poverty, with one in 20 ending up homeless. Because of poor social support, more individuals with schizophrenia become victims than perpetrators of violent crime.
Medications exist but are problematic. The major options today, called antipsychotics, stop all symptoms in only about 20 percent of patients. (Those lucky enough to respond in this way tend to function well as long as they continue treatment; too many, however, abandon their antipsychotic medicines over time, usually because of side effects of schizophrenia medications, a desire to be "normal" or a loss of access to mental health care). Two-thirds gain some relief from antipsychotics yet remain symptomatic throughout life, and the remainder show no significant response.
An inadequate arsenal of medications is only one of the obstacles to treating this tragic disorder effectively. Another is the theories guiding drug therapy. Brain cells (neurons) communicate by releasing chemicals called neurotransmitters that either excite or inhibit other neurons. For decades, theories of schizophrenia have focused on a single neurotransmitter: dopamine. In the past few years, though, it has become clear that a disturbance in dopamine levels is just a part of the story and that, for many, the main abnormalities lie elsewhere. In particular, suspicion has fallen on deficiencies in the neurotransmitter glutamate. Scientists now realize that schizophrenia affects virtually all parts of the brain and that, unlike dopamine, which plays an important role only in isolated regions, glutamate is critical virtually everywhere. As a result, investigators are searching for treatments that can reverse the underlying glutamate deficit.
Multiple Symptoms
To develop better treatments, investigators need to understand how schizophrenia arises--which means they need to account for all its myriad symptoms. Most of these fall into categories termed symptom "positive," "negative" and "cognitive." Positive symptoms generally imply occurrences beyond normal experience; negative symptoms generally connote diminished experience. Cognitive, or "disorganized," symptoms refer to difficulty maintaining a logical, coherent flow of conversation, maintaining attention, and thinking on an abstract level.
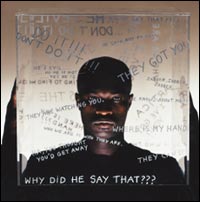
The public is most familiar with the positive symptoms, particularly agitation, paranoid delusions (in which people feel conspired against) and hallucinations, commonly in the form of spoken voices. Command hallucinations, where voices tell people to hurt themselves or others, are an especially ominous sign: they can be difficult to resist and may precipitate violent actions.
Picture: PERCEIVING FRAGMENTS as parts of a whole can be difficult for people with schizophrenia. When normal subjects view fractured images like those above in sequence, they identify the object quickly, but schizophrenic patients often cannot make that leap swiftly.
The negative and cognitive symptoms are less dramatic but more pernicious. These can include a cluster called the 4 A's: autism (loss of interest in other people or the surroundings), ambivalence (emotional withdrawal), blunted affect (manifested by a bland and unchanging facial expression), and the cognitive problem of loose association (in which people join thoughts without clear logic, frequently jumbling words together into a meaningless word salad). Other common symptoms include a lack of spontaneity, impoverished speech, difficulty establishing rapport and a slowing of movement. Apathy and disinterest especially can cause friction between patients and their families, who may view these attributes as signs of laziness rather than manifestations of the illness.
When individuals with schizophrenia are evaluated with pencil-and-paper tests designed to detect brain injury, they show a pattern suggestive of widespread dysfunction. Virtually all aspects of brain operation, from the most basic sensory processes to the most complex aspects of thought are affected to some extent. Certain functions, such as the ability to form new memories either temporarily or permanently or to solve complex problems, may be particularly impaired. Patients also display difficulty solving the types of problems encountered in daily living, such as describing what friends are for or what to do if all the lights in the house go out at once. The inability to handle these common problems, more than anything else, accounts for the difficulty such individuals have in living independently. Overall, then, schizophrenia conspires to rob people of the very qualities they need to thrive in society: personality, social skills and wit.
Beyond Dopamine
|
The emphasis on dopamine-related abnormalities as a cause of schizophrenia emerged in the 1950s, as a result of the fortuitous discovery that a class of medication called the phenothiazines was able to control the positive symptoms of the disorder. Subsequent studies demonstrated that these substances work by blocking the functioning of a specific group of chemical-sensing molecules called dopamine D2 receptors, which sit on the surface of certain nerve cells and convey dopamine's signals to the cells' interior. At the same time, research led by the recent Nobel laureate Arvid Carlsson revealed that amphetamine, which was known to induce hallucinations and delusions in habitual abusers, stimulated dopamine release in the brain. Together these two findings led to the "dopamine theory," which proposes that most symptoms of schizophrenia stem from excess dopamine release in important brain regions, such as the limbic system (thought to regulate emotion) and the frontal lobes (thought to regulate abstract reasoning).
Over the past 40 years, both the strengths and limitations of the theory have become apparent. For some patients, especially those with prominent positive symptoms, the theory has proved robust, fitting symptoms and guiding treatment well. The minority of those who display only positive manifestations frequently function quite well--holding jobs, having families and suffering relatively little cognitive decline over time--if they stick with their medicines.
Yet for many, the hypothesis fits poorly. These are the people whose symptoms come on gradually, not dramatically, and in whom negative symptoms overshadow the positive. The sufferers grow withdrawn, often isolating themselves for years. Cognitive functioning is poor, and patients improve slowly, if at all, when treated with even the best existing medications on the market.
Picture: Objects often have hidden meanings to people with schizophrenia, who may hoard news items, pictures or other things that would seem useless to others. This wall is a re-creation.
Such observations have prompted some researchers to modify the dopamine hypothesis. One revision suggests, for example, that the negative and cognitive symptoms may stem from reduced dopamine levels in certain parts of the brain, such as the frontal lobes, and increased dopamine in other parts of the brain, such as the limbic system. Because dopamine receptors in the frontal lobe are primarily of the D1 (rather than D2) variety, investigators have begun to search, so far unsuccessfully, for medications that stimulate D1 receptors while inhibiting D2s.
In the late 1980s researchers began to recognize that some pharmaceuticals, such as clozapine (Clozaril), were less likely to cause stiffness and other neurologic side effects than older treatments, such as chlorpromazine (Thorazine) or haloperidol (Haldol), and were more effective in treating persistent positive and negative symptoms. Clozapine, known as an atypical antipsychotic, inhibits dopamine receptors less than the older medications and affects the activity of various other neurotransmitters more strongly. Such discoveries led to the development and wide adoption of several newer atypical antipsychotics based on the actions of clozapine (certain of which, unfortunately, now turn out to be capable of causing diabetes and other unexpected side effects). The discoveries also led to the proposal that dopamine was not the only neurotransmitter disturbed in schizophrenia; others were involved as well.
Theories focusing largely on dopamine are problematic on additional grounds. Improper dopamine balance cannot account for why one individual with schizophrenia responds almost completely to treatment, whereas someone else shows no apparent response. Nor can it explain why positive symptoms respond so much better than negative or cognitive ones do. Finally, despite decades of research, investigations of dopamine have yet to uncover a smoking gun. Neither the enzymes that produce this neurotransmitter nor the receptors to which it binds appear sufficiently altered to account for the panoply of observed symptoms.
The Angel Dust Connection
If dopamine cannot account well for schizophrenia, what is the missing link? A critical clue came from the effects of another abused drug: PCP (phencyclidine), also known as angel dust. In contrast to amphetamine, which mimics only the positive symptoms of the disease, PCP induces symptoms that resemble the full range of schizophrenia's manifestations: negative and cognitive and, at times, positive. These effects are seen not just in abusers of PCP but also in individuals given brief, low doses of PCP or ketamine (an anesthetic with similar effects) in controlled drug-challenge trials.
Such studies first drew parallels between the effects of PCP and the symptoms of schizophrenia in the 1960s. They showed, for example, that individuals receiving PCP exhibited the same type of disturbances in interpreting proverbs as those with schizophrenia. More recent studies with ketamine have produced even more compelling similarities. Notably, during ketamine challenge, normal individuals develop difficulty thinking abstractly, learning new information, shifting strategies or placing information in temporary storage. They show a general motor slowing and reduction in speech output just like that seen in schizophrenia. Individuals given PCP or ketamine also grow withdrawn, sometimes even mute; when they talk, they speak tangentially and concretely. PCP and ketamine rarely induce schizophrenia-like hallucinations in normal volunteers, but they exacerbate these disturbances in those who already have schizophrenia.
One example of the research implicating NMDA receptors in schizophrenia relates to the way the brain normally processes information. Beyond strengthening connections between neurons, NMDA receptors amplify neural signals, much as transistors in old-style radios boosted weak radio signals into strong sounds. By selectively amplifying key neural signals, these receptors help the brain respond to some messages and ignore others, thereby facilitating mental focus and attention. Ordinarily, people respond more intensely to sounds presented infrequently than to those presented frequently and to sounds heard while listening than to sounds they make themselves while speaking. But people with schizophrenia do not respond this way, which implies that their brain circuits reliant on NMDA receptors are out of kilter.
If reduced NMDA receptor activity prompts schizophrenia's symptoms, what then causes this reduction? The answer remains unclear. Some reports show that people with schizophrenia have fewer NMDA receptors, although the genes that give rise to the receptors appear unaffected. If NMDA receptors are intact and present in proper amounts, perhaps the problem lies with a flaw in glutamate release or with a buildup of compounds that disrupt NMDA activity.
Some evidence supports each of these ideas. For instance, postmortem studies of schizophrenic patients reveal not only lower levels of glutamate but also higher levels of two compounds (NAAG and kynurenic acid) that impair the activity of NMDA receptors. Moreover, blood levels of the amino acid homocysteine are elevated; homocysteine, like kynurenic acid, blocks NMDA receptors in the brain. Overall, schizophrenia's pattern of onset and symptoms suggests that chemicals disrupting NMDA receptors may accumulate in sufferers' brains, although the research verdict is not yet in. Entirely different mechanisms may end up explaining why NMDA receptor transmission becomes attenuated.
New Schizophrenia Treatment Possibilities
Regardless of what causes NMDA signaling to go awry in schizophrenia, the new understanding--and preliminary studies in patients--offers hope that drug therapy can correct the problem. Support for this idea comes from studies showing that clozapine (Clozaril), one of the most effective medications for schizophrenia identified to date, can reverse the behavioral effects of PCP in animals, something that older antipsychotics cannot do. Further, short-term trials with agents known to stimulate NMDA receptors have produced encouraging results. Beyond adding support to the glutamate hypothesis, these results have enabled long-term clinical trials to begin. If proved effective in large-scale tests, agents that activate NMDA receptors will become the first entirely new class of medicines developed specifically to target the negative and cognitive symptoms of schizophrenia.
The two of us have conducted some of those studies. When we and our colleagues administered the amino acids glycine and D-serine to patients with their standard medications, the subjects showed a 30 to 40 percent decline in cognitive and negative symptoms and some improvement in positive symptoms. Delivery of a medication, D-cycloserine, that is primarily used for treating tuberculosis but happens to cross-react with the NMDA receptor, produced similar results. Based on such findings, the National Institute of Mental Health has organized multicenter clinical trials at four hospitals to determine the effectiveness of D-cycloserine and glycine as therapies for schizophrenia; results should be available this year. Trials of D-serine, which is not yet approved for use in the U.S., are ongoing elsewhere with encouraging preliminary results as well. These agents have also been helpful when taken with the newest generation of atypical antipsychotics, which raises the hope that therapy can be developed to control all three major classes of symptoms at once.
None of the agents tested to date may have the properties needed for commercialization; for instance, the doses required may be too high. We and others are therefore exploring alternative avenues. Molecules that slow glycine's removal from brain synapses--known as glycine transport inhibitors--might enable glycine to stick around longer than usual, thereby increasing stimulation of NMDA receptors. Agents that directly activate "AMPA-type" glutamate receptors, which work in concert with NMDA receptors, are also under active investigation. And agents that prevent the breakdown of glycine or D-serine in the brain have been proposed.
Many Avenues of Attack
Scientists interested in easing schizophrenia are also looking beyond signaling systems in the brain to other factors that might contribute to, or protect against, the disorder. For example, investigators have applied so-called gene chips to study brain tissue from people who have died, simultaneously comparing the activity of tens of thousands of genes in individuals with and without schizophrenia. So far they have determined that many genes important to signal transmission across synapses are less active in those with schizophrenia--but exactly what this information says about how the disorder develops or how to treat it is unclear.
Genetic studies in schizophrenia have nonetheless yielded intriguing findings recently. The contribution of heredity to schizophrenia has long been controversial. If the illness were dictated solely by genetic inheritance, the identical twin of a schizophrenic person would always be schizophrenic as well, because the two have the same genetic makeup. In reality, however, when one twin has schizophrenia, the identical twin has about a 50 percent chance of also being afflicted. Moreover, only about 10 percent of first-degree family members (parents, children or siblings) share the illness even though they have on average 50 percent of genes in common with the affected individual. This disparity suggests that genetic inheritance can strongly predispose people to schizophrenia but that environmental factors can nudge susceptible individuals into illness or perhaps shield them from it. Prenatal infections, malnutrition, birth complications and brain injuries are all among the influences suspected of promoting the disorder in genetically predisposed individuals.
Over the past few years, several genes have been identified that appear to increase susceptibility to schizophrenia. Interestingly, one of these genes codes for an enzyme (catechol-O-methyltransferase) involved in the metabolism of dopamine, particularly in the prefrontal cortex. Genes coding for proteins called dysbindin and neuregulin seem to affect the number of NMDA receptors in brain. The gene for an enzyme involved in the breakdown of D-serine (D-amino acid oxidase) may exist in multiple forms, with the most active form producing an approximately fivefold increase in risk for schizophrenia. Other genes may give rise to traits associated with schizophrenia but not the disease itself. Because each gene involved in schizophrenia produces only a small increase in risk, genetic studies must include large numbers of subjects to detect an effect and often generate conflicting results. On the other hand, the existence of multiple genes predisposing for schizophrenia may help explain the variability of symptoms across individuals, with some people perhaps showing the greatest effect in dopamine pathways and others evincing significant involvement of other neurotransmitter pathways.
Finally, scientists are looking for clues by imaging living brains and by comparing the brains of people who have died. In general, individuals with schizophrenia have smaller brains than unaffected individuals of similar age and sex. Whereas the deficits were once thought to be restricted to areas such as the brain's frontal lobe, more recent studies have revealed similar abnormalities in many brain regions: those with schizophrenia have abnormal levels of brain response while performing tasks that activate not only the frontal lobes but also other areas of the brain, such as those that control auditory and visual processing. Perhaps the most important finding to come out of recent research is that no one area of the brain is "responsible" for schizophrenia. Just as normal behavior requires the concerted action of the entire brain, the disruption of function in schizophrenia must be seen as a breakdown in the sometimes subtle interactions both within and between different brain regions.
Because schizophrenia's symptoms vary so greatly, many investigators believe that multiple factors probably cause the syndrome. What physicians diagnose as schizophrenia today may prove to be a cluster of different illnesses, with similar and overlapping symptoms. Nevertheless, as researchers more accurately discern the syndrome's neurological bases, they should become increasingly skilled at developing treatments that adjust brain signaling in the specific ways needed by each individual.
APA Reference
Staff, H.
(2004, March 13). Decoding Schizophrenia, HealthyPlace. Retrieved
on 2026, January 7 from https://www.healthyplace.com/thought-disorders/schizophrenia-articles/decoding-schizophrenia